Abstract
Abstract 1532
Patient readmission within 30 days from discharge has been perceived by Centers for Medicare and Medical Services as an indicator of poor health-care quality for specific high-cost medical conditions. Patients who undergo allogeneic hematopoietic stem cell transplantation (AlloHSCT) were previously found to have higher rates of readmission as compared to those with autologous HSCT. The purpose of this exploratory retrospective study was to identify the reasons and risk factors for 30-days readmission among the recipients of myeloablative AlloHSCT.
618 adults were at risk for 30-day readmission following AlloHSCT from 1990 to 2009 at our single academic institution. Recursive partitioning analysis was used to identify the most optimal grouping of various preparative regimens relative to readmission. Univariate and multivariable risk factors for readmission were identified with logistic regression analysis. Impact of 30-day readmission on overall mortality was estimated by Cox proportional hazards analysis.
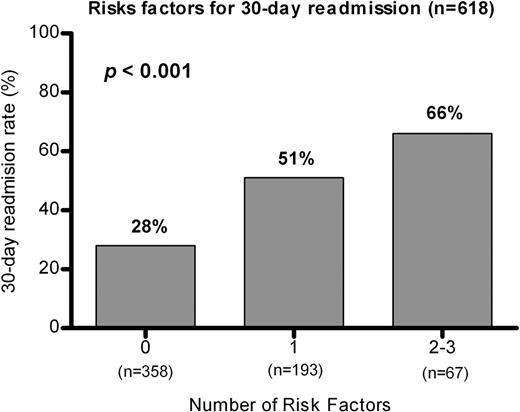
242 (39%) of 618 patients (median age=42 years [range, 18–66]; 54% males; 89% Caucasians) were readmitted after a median of 10 days (range, 1–30) from discharge. Median duration of readmission was 8 days (range, 0–103). Infections (n=68), fever without identified source of infection (n=63), gastrointestinal complications (n=44), GVHD (n=38), and other reasons (n=29) accounted for 28%, 26%, 18%, 16%, and 12% of readmissions, respectively. 30% of readmitted patients had lymphoid and 67% had myeloid malignancy; 90% received ≥1 prior chemotherapy; 26% had TBI-containing preparative regimen; bone marrow was the most common (84%) source of stem cells; 46% had unrelated donor AlloHCST. During their index admission, 65% of subsequently readmitted patients were hospitalized for more than 29 days; 52% of patients recovered their ANC > 500/mL within 15 days; 41% had infection; 16% had grade II-IV GVHD. In univariate analysis, greater risk for readmission was associated with lymphoid malignancy (vs. myeloid, p=0.03), more previous chemotherapy regimens (p=0.01), TBI-containing preparative regimen (p<0.001), peripheral stem cell source (vs. bone marrow, p=0.01), unrelated donor (p<0.001), and infection during admission for AlloHSCT (p<0.001). In multivariable analysis, TBI-based preparative regimen (HR=2.6; 95% CI, 1.6–4.2), infection during admission for AlloHSCT (HR=2.3; 95% CI, 1.6–3.3), and peripheral stem cell source (vs. bone marrow, HR=1.9; 95% CI, 1.03–3.4) predicted 30-day readmission. 30-day readmission was an independent predictor of all-cause mortality (HRAdj=1.8; 95% CI, 1.5–2.2).
30-day hospital readmissions following myeloablative AlloHSCT portended poor survival. Our data emphasize the importance of risk-standardized approach to 30-day hospital readmission if it is used as a quality-of-care metric for bone marrow transplantation. Further studies will be necessary to validate our findings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.