Abstract
Abstract 217
HCT is used with curative intent in children with cancer at risk for relapse. Improvements in transplantation strategies have contributed to increments in survival approximating 10% per decade. Adult HCT survivors are at increased risk for chronic health conditions (Sun, Blood 2010). The magnitude of risk of these conditions in childhood HCT survivors compared with the general population is not defined. Furthermore, while children treated with conventional therapy carry a substantial burden of morbidity (Oeffinger, N Engl J Med 2006), little data exists regarding the added impact of HCT-related conditioning and GvHD on the prevalence of chronic health conditions and functional status.
Participants were drawn from two studies: BMTSS and CCSS. BMTSS examined long-term outcomes in individuals undergoing HCT between 1976 and 1998 at City of Hope or University of Minnesota. Participants were ≤21 years of age at diagnosis of AML, ALL, HL, and NHL, had survived at least 5 yrs from primary diagnosis and 2 yrs from myeloablative HCT. CCSS is a multi-institutional cohort of five-year survivors of childhood cancer diagnosed between 1970 and 1986, and their siblings. For the current study, participation was limited to those treated conventionally with the same diagnoses as BMTSS. Participants for both studies had completed a questionnaire covering the following areas: presence of physical health conditions (endocrinopathies; central nervous system compromise; cardiopulmonary dysfunction; gastrointestinal sequelae; musculoskeletal abnormalities; and subsequent malignancies); chronic GvHD (BMTSS); and sociodemographics. Responses obtained from BMTSS were compared to conventionally treated childhood cancer survivors and sibling controls enrolled in CCSS. Chronic physical health conditions were graded using CTCAE v 3.0 (grade 1–4, ranging from mild to life-threatening/ disabling). Relative risk regression was used to identify risk of health conditions (RR) and 95% confidence interval (CI).
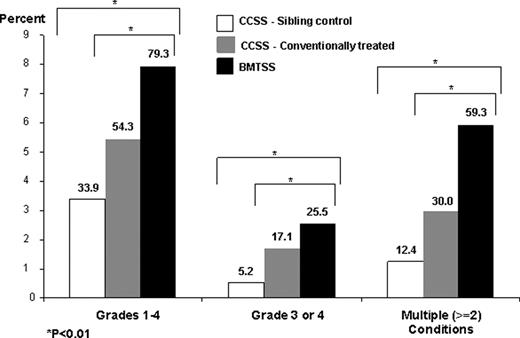
The current study included 145 BMTSS participants, 4,020 siblings, and 7,207 CCSS cancer survivors. Median age at participation – BMTSS: 24 yrs; childhood cancer survivors: 24.6 yrs; siblings: 26.6; time from diagnosis – BMTSS: 11.9 yrs; CCSS: 15.6 yrs. 79.3% of BMTSS participants reported at least one condition (grades 1–4); 59.3% multiple (≥2); and 25.5% severe or life-threatening conditions (grade 3–4). Prevalence and severity of these conditions was significantly greater for BMTSS when compared with cancer survivors or siblings (Figure). BMTSS vs. Siblings: After adjustment for age at questionnaire, gender, and ethnicity, BMTSS participants were significantly more likely than sibling controls to report chronic health conditions: grades 1–4: RR=2.7 (95% CI, 2.4–3.0, p<0.01); grades 3–4: RR=6.4 (4.6-8.8, p<0.01); multiple conditions: RR=5.9 (5.0-7.0, p<0.01). In addition, BMTSS participants were significantly more likely to report compromised functional status: adverse general health: RR=3.4 (2.1-5.3, p<0.01); activity limitations: RR=6.8 (5.0-9.3, p<0.01); and functional impairment: RR=7.8 (5.1-12.0, p<0.01). BMTSS vs. CCSS cancer survivors: After adjustment for age, follow-up, gender, ethnicity/race, diagnosis, pre-HCT therapeutic exposures (dose-specific chemotherapy, radiation), and treatment era, BMTSS participants were 1.5 (1.3-1.7, p<0.01) times as likely as conventionally treated patients to report a chronic condition; 2.3 (1.5-3.5, p<0.01) times as likely to report severe/ life-threatening conditions; and 2.2 (1.7-2.8, p<0.01) times as likely to report multiple conditions. Allogeneic HCT recipients with a history of chronic GvHD were at a modestly higher risk of reporting multiple chronic health conditions (Table).
| . | RR (95% CI) Grades 1-4 . | RR (95% CI) Grade 3 or 4 . | RR (95% CI) Multiple (≥2) Conditions . |
|---|---|---|---|
| Conventionally treated (CCSS) | 1.0 | 1.0 | 1.0 |
| Autologous HCT (BMTSS) | 1.3 (1.0–1.7) | 1.7 (0.7–3.9) | 1.5 (0.9–2.2) |
| Allogeneic HCT, no GvHD (BMTSS) | 1.5 (1.2–1.7) | 2.5 (1.6–3.9) | 2.2 (1.7–2.8) |
| Allogeneic HCT, GvHD (BMTSS) | 1.7 (1.4–2.0) | 2.7 (1.3–5.3) | 2.9 (2.1–3.9) |
| . | RR (95% CI) Grades 1-4 . | RR (95% CI) Grade 3 or 4 . | RR (95% CI) Multiple (≥2) Conditions . |
|---|---|---|---|
| Conventionally treated (CCSS) | 1.0 | 1.0 | 1.0 |
| Autologous HCT (BMTSS) | 1.3 (1.0–1.7) | 1.7 (0.7–3.9) | 1.5 (0.9–2.2) |
| Allogeneic HCT, no GvHD (BMTSS) | 1.5 (1.2–1.7) | 2.5 (1.6–3.9) | 2.2 (1.7–2.8) |
| Allogeneic HCT, GvHD (BMTSS) | 1.7 (1.4–2.0) | 2.7 (1.3–5.3) | 2.9 (2.1–3.9) |
Childhood HCT survivors carry a significantly higher burden of morbidity when compared with the general population, as well as children treated with conventional therapy, providing evidence for a critical need for close monitoring of this high-risk population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.