Abstract
Abstract 2386
Acute myeloid leukemia (AML) with chromosomal translocation (6;9)(p23;q34) results in a chimeric fusion gene between DEK/NUP214 (formerly DEK/CAN), and is a rare disease, accounting for approximately 1% of cases. This entity is considered to be a good indication for allogeneic hematopoietic stem cell transplantation (allo-HSCT) due to its poor prognosis and non-responsiveness to chemotherapy. However, whether the prognosis of patients with exclusive DEK/NUP214 abnormality is improved by allo-HSCT has not been demonstrated. We conducted a retrospective study to examine the outcomes of allo-HSCT in AML patients with the DEK/NUP214 gene using the databases of the Japan Society for Hematopoietic Cell Transplantation (JSHCT) and the Japan Cord Blood Bank Network (JCBBN).
We identified de novo AML patients who underwent transplant between January 1996 and December 2007 with no prior treatment by allo-HSCT. Clinical features and outcomes of the patients with DEK/NUP214 abnormality and 3 different control groups (patients with chromosome 7 abnormalities, complex karyotype or normal karyotype) were compared.
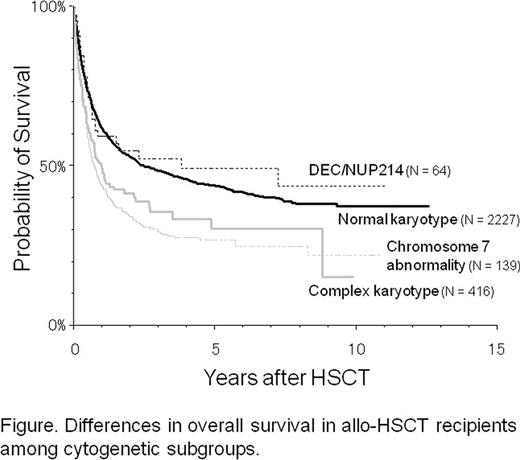
Of 4517 AML cases meeting the above criteria, the number of patients with normal karyotype, chromosome 7 abnormalities, complex karyotype and DEK/NUP214 abnormality was 2227, 139, 416 and 64, respectively. The median age of each group was 41, 37, 41 and 34 years, respectively; patients with the DEC/NUP214 abnormality were significantly younger than those with the complex karyotype, and patients with normal chromosomes. Gender was not biased among the groups. Overall survival (OS) of the patients with DEC/NUP214 abnormality at 5 years was 49%, which was superior to the OS of the patients with normal karyotype, chromosome 7 abnormalities and complex karyotype (44%, 30% and 27%, respectively; P < 0.0001; Figure). This trend was significant in HSCT grafts with bone marrow and peripheral blood stem cells. In patients with DEK/NUP214 abnormality, none of the following factors improved survival; combination of gender between patient-donor, dose of total body irradiation prior to HSCT; and use of prophylactic immunosuppressants for graft-versus-host disease. However, the status at HSCT had a significant impact on outcome (5-year OS: 66% in patients in complete remission (CR) at HSCT vs. 31% in non-CR patients; P < 0.001). Analysis exclusively for the patients in CR at HSCT showed similar results as above.
Difference in overall survival in allo-HSCT recipients among cytogenetic subgroups
Difference in overall survival in allo-HSCT recipients among cytogenetic subgroups
Our results suggest that patients with the DEK/NUP214 abnormality are more likely to respond to allo-HSCT. Allo-HSCT should be particularly recommended for patients experiencing CR after prior remission-induction chemotherapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.