Abstract
Abstract 2438
Abnormalities of VWF have been described in WM pts, and several cases of AVWS have been reported. We aimed to describe the frequency of AVWS and the distributions of von Willebrand factor Ristocetin Cofactor activity (VWF:RCo) and antigen (VWF:Ag) levels along with VEGF expression in WM pts.
We systematically assessed both levels of VWF:Rco and VWF:Ag in a series of 72 WM pts (median age: 70 years, 39 to 91 years, sex ratio M/F: 1.6, symptomatic: 55). Diagnostic and treatment criteria for WM fulfilled recommendations of the 2nd international WM workshop. AVWS was suspected when VWF:RCo level was <50% (40% for blood group O pts). Immunostainings for vascular endothelial growth factor (VEGF) and VWF with assessment of microvessel density (MVD) were performed in 23 pts.
Mean levels of VWF:Ag and VWF:RCo were 167% and 152% respectively, with a significant negative relationship between both VWF:RCo and VWF:Ag and serum M-component concentration in WM pts with VWF:Ag <130% (p<1×10−4 and p=0.006, respectively).
AVWS was suspected in 10 pts with symptomatic WM (median level of VWF:RCo: 31%, Haemorrhage in 4 pts). Pts with suspected AVWS had higher serum monoclonal IgM (mIgM) concentration than remaining pts (p=0.001). Reduction of IgM with plasmapheresis (4 pts) or treatment of WM was associated with an increase in VWF:Ag and VWF:RCo levels. High level of propeptide and increase in the ratio propeptide/VWF suggested an increase in the clearance of mature VWF. However, IgM inhibitory activity was absent in all evaluated pts with suspected AVWS (n=6). VWF immunostaining on bone marrow trephine biopsy did not support an adsorption of VWF on tumoral cells.
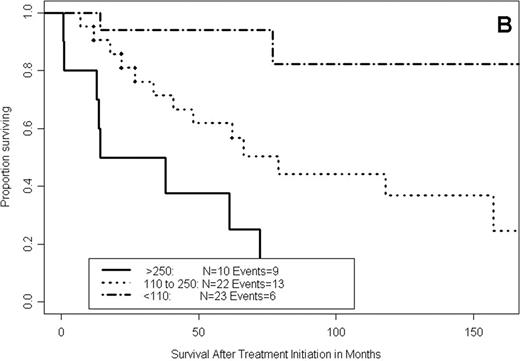
Pspline proportional hazard regression models including VWF:Ag (p=10−4) and recursive partitioning analyses of survival showed an increase in the hazard for death with the increase in the level of VWF:Ag. Thus, 43 pts (59%) presented with VWF:Ag > 110%, and among these, 13 pts with VWF:Ag > 250%. They had higher level of propeptide (p=0.0006) than pts without abnormality of VWF (VWF:Ag < 110% and no AVWS) but the ratio propeptide/VWF:Ag was not significantly different between both subgroups, suggesting the presence of a chronic endothelial activation. Immunostainings identified a high MVD in 6 of the 23 tested pts, the presence of VEGF on mast cells in 8 pts and on tumoral cells in 13 pts. Pts with high MVD and pts expressing VEGF on mast cells had significantly higher levels of VWF:Ag than other pts (p=0.05 and 0.01 respectively). These pts more frequently had VWF:Ag levels above 250% (2-sided Fisher test: p=0.004 and 0.006 respectively). In addition, pts with high MVD more frequently (p=0.05) expressed VEGF on mast cells than other pts. The 5-year survival of pts with VWF:Ag < 110%, between 110% and 250% and >250% were 96%, 71%, and 44% respectively (p<0.0001, figure A). High VWF:Ag was also a significant adverse prognostic factor for survival after first-line therapy (p<0.0001, figure B), independently of international scoring system (p≤0.001), and for survival after sampling (p<0.0001).
Taken together, our results support a systematic assessment of VWF:RCo and VWF:Ag in WM pts. Follow-up data supported the importance of the treatment of WM in the management of suspected AVWS. Systematic assessment identified up to 59% of high-risk pts with high level VWF:Ag. The identification of this new prognostic factor raised new issues on the underlying cellular interactions between tumoral cells, mast cells and endothelial cells in WM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.