Abstract
Abstract 257
Advances in treatment of thalassemia have led to increased life expectancy for patients making outcomes such as health related quality of life (HRQOL) an important consideration of therapy. Little has been published about the HRQOL of pediatric patients with thalassemia. There are limited reports on how this illness impacts the family. Because the familial situation is the starting point for how patients learn to live with their condition, it is important to document this effect and how it changes over time. This report looks at changes in parental reported HRQOL from baseline (BL) to year 1 (Y1) in the Thalassemia Clinical Research Networks (TCRN) Thalassemia Longitudinal Cohort (TLC) study.
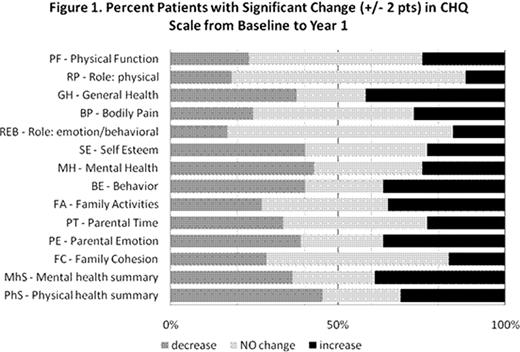
The TCRN is a NIH-sponsored network of 16 major thalassemia centers in the US, Canada and London. We report here on the results from 77 patients under the age of 14 who completed BL and assessments at Y1. Overall the patients were 47% male with a mean age of 9 years (range 5–13). 94% were chronically transfused, and 69% had β-thalassemia, and 12% were E-β thalassemia patients. 57% used an oral chelator, while 29% were on desferoxamine (DFO). HRQOL was measured by self-report with the Children Health Questionnaire (CHQ), 28-item Parental Form (PF28). The 28 items derive 12 subscales that assess physical and psychosocial health. 2 summary scales assess overall physical health and psychosocial health. We defined a clinically significant change as a difference of at least 2 points on any subscale.
Clinical Changes: 45% saw a reduced number of transfusions from BL to year 1 (32% showed no change). 73% did not change chelator, while 18% changed from DFO to oral (2.6% other way). 5% began a chelation regimen. Only one percent of patients developed new secondary complications. 63% showed no change in their general adherence rate; 25% showed a decrease. HRQOL changes: As a population, mean HRQOL remained stable over the 1 year study period. Age appears to be significant for CHQ assessment of child's self esteem and behavior (and overall psychosocial assessment), but gender, country and ethnicity do not appear to be significant. The average number of scales with significant changes was eight. Only one CHQ assessment does not show any significant changes on any CHQ scale, while three reports showed changes on all 14 scales. The psychosocial scales showed more significant changes than physical health assessments. Figure 1 illustrates the reported changes by scale. Measures of overall general health, parental emotions and child behavior showed the most changes. Assessment of the child's physical and psychosocial roles and family cohesion showed the least change. The physical health assessments of function and pain showed lower significant changes than the psychosocial health assessments. More psychological health measures show a significant drop than familial assessments. When we examine scale changes by age groups, the youngest age group (5-7) showed modestly better physical and psychosocial scale changes. The 8–10 age group saw more than twice the number of parents seeing a decline in a physical or psychosocial health scale. The oldest age group (11-14) showed the fewest changes, with mainly higher physical health scale changes, but lower scores on the psychosocial scales. Clinical Associations: Changes in number of transfusions and adherence do not appear to impact CHQ assessment. However, changes in chelator appear to be significant for parental time (P=0.048) and the psychosocial summary scale (p=0.04). Changes in secondary complication appear to be associated with changes in the CHQ assessment of the child's behavior (p=.04).
The dearth of clinical changes suggests that patients enrolled in TCRN are receiving optimized health care. The lack of changes on the CHQ's physical health scales is to be expected given the low number of clinical changes, and the reported changes in CHQ do not appear to be related to clinical changes. At this stage of data analysis, CHQ assessment in thalassemia appears to be associated with the normal effects a growing child has on the family. This would be the desired result of effective clinical intervention in thalassemia. Further analyses of changes are needed to understand the relationship between changes in HRQOL and specific changes in clinical measures.
Neufeld:Novartis, Inc: Research Funding; Ferrokin, Inc: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.