Abstract
Abstract 3295
WT1 (Wilms' tumor gene 1) encodes a transcription factor, which regulates various types of genes and plays an important role in cell proliferation and differentiation. WT1 is highly expressed in leukemia and various types of solid tumors. In vivo immunization of mice with MHC class I-restricted 9-mer WT1 peptide elicited WT1-specific cytotoxic T lymphocytes (CTLs) and rejected WT1-expressing leukemia cells, demonstrating that WT1 is a tumor rejection antigen. Next, identification of human HLA class I-restricted WT1 peptides was performed, and WT1 235 (235-243 aa) and WT1 126 (126-134 aa) were determined as an HLA-A*2402- or HLA-A*0201- restricted WT1 peptide, respectively, by using in vitro WT1-specific CTL induction assay.
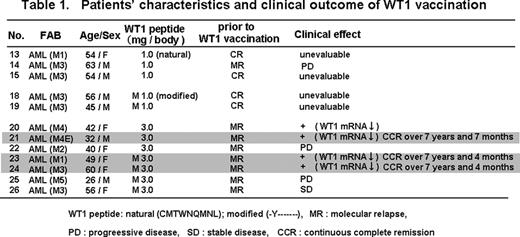
On the basis of these fundamental experiments, we performed for the first time a phase I clinical trial of WT1 peptide immunotherapy with the approval of our ethical committee. A total of 26 patients with acute myeloid leukemia (AML), myelodysplastic syndrome, breast or lung cancer were intradermally injected with a HLA-A*2402-restricted natural or modified 9-mer WT1 peptide emulsified with Montanide ISA51 adjuvant at 0.3, 1.0 or 3.0 mg at 2-week intervals. As shown in Table1, 12 AML patients were WT1-vaccinated and eight of the 12 AML patients were evaluable for clinical effect because of the existence of minimal residual disease (MRD) assessed by WT1 mRNA assay. Since four of the eight patients had obvious clinical response with the decrease in WT1 mRNA within three injections of WT1 vaccine, WT1 vaccination was repeated for them afterward (in the case that clinical response was not obvious within three injections of WT1 vaccine, WT1 vaccination was discontinued). However, one patient (No. 20) had re-increase in WT1 mRNA and WT1 vaccination was discontinued. The remaining three patients (Nos. 21, 23 and 24) have been repeatedly receiving WT1 vaccination (intervals were changed from 2 weeks to one month) over 7 years until now. WT1 mRNA levels, which directly reflected the amount of leukemic blast cells, were abnormally high and 102-103 copies/mg RNA in PB (normal level is < 50 copies/mg RNA) before WT1 vaccination in these three AML patients, showing that the patients were at molecular relapse with MRD. In nos. 21 and 23 patients, a decrease and increase in WT1 mRNA levels were repeated during early stages of WT1 vaccination. However, afterward, WT1 mRNA levels gradually decreased and reached normal level approximately three and a half years after the beginning of WT1 vaccination and have been maintained at normal level until now. In patient no. 24, high levels of WT1 mRNA (near 103 copies) gradually decreased by repeated WT1 vaccination and returned to normal level approximately 5 years after the beginning of WT1 vaccination although it was much delayed. Thus, these three patients had achieved continuous complete remission regardless of high risk for clinical relapse.
WT1-specific immune responses were evaluated by WT1 tetramer assay. Frequencies of WT1-specific cytotoxic T lymphocytes (CTLs) (WT1 tetramer+ CD8+ T cells) in the patients were already higher before WT1 vaccination, compared to those in healthy volunteers, which was a frequent phenomenon in WT1-expressing tumor-bearing patients, but the WT1-specific CTLs were a IFN-g− inactivated form. After WT1 vaccination, a IFN- g+ activated from of WT1-specific CTLs appeared and was maintained until now.
No adverse effects except local erythema and eruption at the injection sites of WT1 vaccine were observed regardless of repeated long-term WT1 vaccination over 7 years. These finding indicated that WT1-specific CTLs could attack WT1-expressing leukemic blast cells but ignored WT1-expressing normal cells such as podocytes of kidney and progenitor cells of various types of organs.
In conclusion, we presented here the first report of promising clinical outcome of very long-term WT1 vaccination for AML patients with high risk for relapse. WT1 peptide immunotherapy should have good prospects as a cure-oriented therapy for AML and could be the first choice of the treatments for AML patients who had still MRD after induction chemotherapy, especially for elder patients who were intolerable to intensive chemotherapy. WT1 peptide immunotherapy may be also a better choice of treatments for AML patients who have high risk for relapse but are intolerable to allogeneic hematopoietic stem cell transplantation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.