Abstract
Abstract 4136
The serum free light chain (FLC) assay quantitates free kappa and free lambda immunoglobulin light chains. This assay has prognostic value in MGUS, multiple myeloma (MM), solitary plasmacytoma, and amyloid light chain (AL) amyloidosis, and has been incorporated in response criteria for both MM and AL amyloidosis. We previously showed elevated FLC was associated with poor outcome in diffuse large B-cell lymphoma (DLBCL) patients from a phase II cooperative group clinical trial (Blood (ASH Annual Meeting Abstracts) 2009 November 20, 2009; 114(22): 136). Here we replicate those findings in a large clinic based epidemiology cohort, as well as examine FLC abnormalities in other lymphoma subtypes.
Newly diagnosed lymphoma patients were prospectively enrolled in the University of Iowa/Mayo Clinic SPORE Molecular Epidemiology Resource (MER). Serum FLC was quantitated from enrollment research serum draws within 9 months of diagnosis using the Freelite FLC assay (The Binding Site, Ltd., Birmingham, UK). Elevated FLC was defined as either kappa or lambda above the published reference range. Monoclonal elevated FLC was defined as elevated FLC with an abnormal FLC ratio; polyclonal elevated FLC was defined as elevated FLC with an FLC ratio in the normal reference range. Clinical data was abstracted using a standard protocol for the MER and patients were followed systematically for event-free (progression, retreatment, or death due to any cause) and overall survival (EFS and OS, respectively). Cox proportional hazards models were used to evaluate the unadjusted association between FLC and outcome.
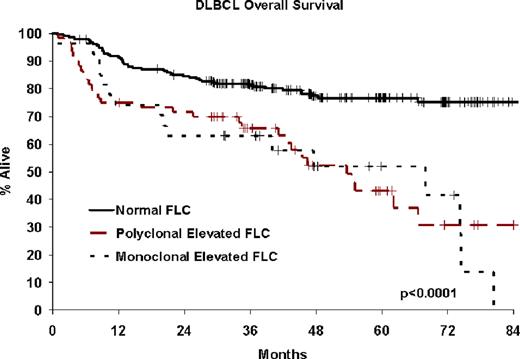
1118 lymphoma patients diagnosed between September 2002 and February 2008 with available serum were assayed. At a medium follow-up of 49 months (range 1–94), 484 patients (43%) had an event and 249 patients died (22%). Elevated FLC was present in 27% of lymphomas, with prevalence ranging from 13% in follicular lymphoma (FL) to 64% for mantle cell lymphoma (MCL) and 77% for lymphoplasmacytic lymphoma. Elevated FLC was present in 27% of DLBCL and associated with poor EFS (monoclonal hazard ratio (HR)=2.56, polyclonal HR=1.99, all p<0.001) and OS (monoclonal HR=3.22, polyclonal HR=2.91, all p<0.0001), replicating our previous findings. Elevated FLC was generally polyclonal (FLC ratio normal) across lymphoma subtypes, though monoclonal elevated FLC (FLC ratio abnormal) was common in MCL and the post-follicular lymphomas. Elevated FLC was associated with inferior EFS in all lymphomas combined (monoclonal HR=1.92, 95% CI:1.44-5.55, polyclonal HR=1.38, 95% CI:1.09-1.74); this association remained consistent in most subtypes (see table). In addition, elevated FLC was associated with poor EFS in MCL (monoclonal) and Hodgkin lymphoma (HL; polyclonal). Elevated FLC was also significantly associated with OS in HL (polyclonal HR=6.24, 95% CI 2.44–15.9), FL (polyclonal HR=5.85, 95% CI 2.62–13.0), post follicular lymphomas (polyclonal HR=4.16, 95% CI 1.17–14.8), as well as for all lymphomas combined (monoclonal HR=2.24, 95% CI 1.52–3.29, polyclonal HR=2.33, 95% CI 1.74–3.11).
A significant percentage of lymphoma patients have elevated FLC. Our previous discovery of elevated FLC predicting poor outcome in DLBCL was confirmed in a large, independent dataset. Prevalence and type of elevated FLC (monoclonal vs. polyclonal) varies by lymphoma subtype. Elevated monoclonal and polyclonal FLC is associated with poor outcome broadly in lymphoma, as well as specifically for a number of lymphoma subtypes, supporting FLC as a potentially useful prognostic biomarker in many lymphoma subtypes.
| Lymphoma Subtype . | N . | Elevated FLC . | Monoclonal Elevated FLC . | EFS Unadjusted HR (95% CI) . | Polyclonal Elevated FLC . | EFS Unadjusted HR (95% CI) . |
|---|---|---|---|---|---|---|
| DLBCL | 322 | 27.0% | 8.4% | 2.56 (1.49, 4.40) | 18.6% | 1.99 (1.32, 3.02) |
| Follicular | 280 | 13.2% | 4.3% | 1.11 (0.49, 2.53) | 8.9% | 1.57 (0.90, 2.74) |
| Mantle Cell | 74 | 63.5% | 24.3% | 2.78 (1.33, 5.74) | 39.2% | 1.25 (0.62, 2.51) |
| T-Cell | 67 | 38.8% | 3.0% | NA | 35.8% | 0.70 (0.39, 1.29) |
| Post Follicular | 107 | 40.2% | 19.6% | 1.66 (0.83, 3.35) | 20.6% | 1.42 (0.69, 2.91) |
| Splenic/Nodal MZL | 19 | 42.1% | 21.1% | NA | 21.1% | NA |
| MALT | 70 | 30.0% | 10.0% | 1.45 (0.42, 4.98) | 20.0% | 1.62 (0.67, 3.93) |
| LPL | 18 | 77.8% | 55.6% | NA | 22.2% | NA |
| Hodgkin Lymphoma | 145 | 24.8% | 0.7% | NA | 24.1% | 3.00 (1.46, 6.18) |
| All B-cell NHL | 869 | 26.7% | 10.1% | 2.08 (1.54, 2.81) | 16.6% | 1.49 (1.14, 1.94) |
| All lymphoma | 1118 | 27.1% | 8.6% | 1.92 (1.44, 2.55) | 18.5% | 1.38 (1.09, 1.74) |
| Lymphoma Subtype . | N . | Elevated FLC . | Monoclonal Elevated FLC . | EFS Unadjusted HR (95% CI) . | Polyclonal Elevated FLC . | EFS Unadjusted HR (95% CI) . |
|---|---|---|---|---|---|---|
| DLBCL | 322 | 27.0% | 8.4% | 2.56 (1.49, 4.40) | 18.6% | 1.99 (1.32, 3.02) |
| Follicular | 280 | 13.2% | 4.3% | 1.11 (0.49, 2.53) | 8.9% | 1.57 (0.90, 2.74) |
| Mantle Cell | 74 | 63.5% | 24.3% | 2.78 (1.33, 5.74) | 39.2% | 1.25 (0.62, 2.51) |
| T-Cell | 67 | 38.8% | 3.0% | NA | 35.8% | 0.70 (0.39, 1.29) |
| Post Follicular | 107 | 40.2% | 19.6% | 1.66 (0.83, 3.35) | 20.6% | 1.42 (0.69, 2.91) |
| Splenic/Nodal MZL | 19 | 42.1% | 21.1% | NA | 21.1% | NA |
| MALT | 70 | 30.0% | 10.0% | 1.45 (0.42, 4.98) | 20.0% | 1.62 (0.67, 3.93) |
| LPL | 18 | 77.8% | 55.6% | NA | 22.2% | NA |
| Hodgkin Lymphoma | 145 | 24.8% | 0.7% | NA | 24.1% | 3.00 (1.46, 6.18) |
| All B-cell NHL | 869 | 26.7% | 10.1% | 2.08 (1.54, 2.81) | 16.6% | 1.49 (1.14, 1.94) |
| All lymphoma | 1118 | 27.1% | 8.6% | 1.92 (1.44, 2.55) | 18.5% | 1.38 (1.09, 1.74) |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.