Abstract
Abstract 4401
16 million units of pRBCs were transfused in the United States in 2006. The number of units transfused increases by 5–7% yearly, although the number of donated units has not increased proportionally leading to increasing shortages. The regional blood banks are responsible for the majority of collections. They typically communicate with hospital blood banks and distribute blood to match predicted needs. The hospital blood banks communicate with hospital administration and ordering physicians about shortages and may recommend strategies to decrease usage. Although the overall blood transfused decreases during a shortage, the effect of a shortage on physician prescribing behavior has not been studied. We randomized critical care physicians in an experimental survey design to understand the effect of varying levels of pRBC shortage on their prescription of blood products.
We used an experimental survey design to assess changes in critical care physicians' pRBC transfusion threshold during times of varying scarcity. 1,940 Critical care physicians received two clinical scenarios, varying only whether there was a hospital wide shortage of blood products, a regional shortage, or no shortage. The vignette stated: “You are the primary physician for this patient. The patient is a 54 year old woman with dark, heme positive stools who is otherwise asymptomatic and is hemodynamically stable.” The physicians were asked whether they would initiate transfusion at 5 different hgb/hct levels from 5g/dl/15% to 10g/dl/30% and the number of units they would transfuse.
| Version . | Shortage Scenario #1 . | Shortage Scenario #2 . |
|---|---|---|
| 1 | None | Hospital |
| 2 | Hospital | None |
| 3 | Hospital | Regional |
| 4 | Regional | Hospital |
| 5 | None | Regional |
| 6 | Regional | None |
| Version . | Shortage Scenario #1 . | Shortage Scenario #2 . |
|---|---|---|
| 1 | None | Hospital |
| 2 | Hospital | None |
| 3 | Hospital | Regional |
| 4 | Regional | Hospital |
| 5 | None | Regional |
| 6 | Regional | None |
Participants also responded to specific questions about personal and practice characteristics, attitude scales and transfusion practices.
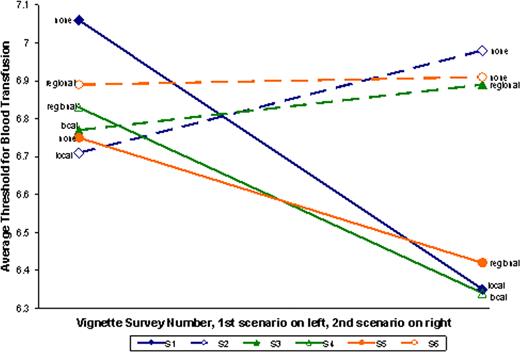
Survey respondents (n= 575, response rate 30%) significantly changed their transfusion threshold based on changing shortage scenarios. Order effects were demonstrated in all surveys where the respondent was presented with a less severe shortage scenario followed by a more severe shortage scenario.
Single unit transfusions were utilized by 54.1% of respondents at their transfusion threshold. The percentage of physicians transfusing single units increased substantially in each of the versions that went from less serious to more serious shortage vignettes. In response to statements about allocation of resources, a majority of physicians endorsed the need for rationing (73.4%). A majority also expressed the view that individual physicians are not capable of allocating scarce resources fairly (55.1%).
This study has three main findings. First, the respondents revealed progressively more restricted use of pRBC transfusions in the setting of progressively more proximate shortages of blood products. This finding suggests that physicians attend to information about shortages and in these scenarios, are willing to change their transfusion practices with individual patients in ways that reflect the needs of other patients. Second, these observed effects were substantially altered by the order of presentation of scenarios. Physicians often became stricter about their use of blood products when told about a shortage or a more proximate shortage, but they did not become more relaxed when later told about no shortage, or a more distant shortage. These findings suggest that continued reminders about scarcity might make physicians thriftier in their use of blood products. Third, physician's revealed use of blood products in response to hypothetical scenarios corresponds to more general feelings about rationing determined from their responses to attitude scales.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.