Abstract
Abstract 4969
Hypomethylating agents have recently been shown to prolong overall survival and improve quality of life in patients with INT-2 and high IPSS risk myelodysplasia (MDS) and low bone marrow blast count acute myeloid leukemia (AML).
Since September 2008 we have been treating 26 patients affected by acute myeloid leukemia (13 patients), MDS (11 patients) or chronic myelomonocytic leukemia (2 patients) with 5-azacitidine.
According to recent guidelines, most of myelodysplastic patients eligible for treatment belonged to the IPSS INT-2 or high risk groups. Patients with acute myeloid leukemia had a medullary blast count of 20–30%, except for four cases. Patients with chronic myelomonocytic leukemia had a medullary blast count > 10% and < 20%. The median age of patients when treatment was started was 69,5 years (range: 51–82). Azacitidine was administered subcutaneously (75 mg/m2/d) for 7 days of every 28-day cycle until loss of response or disease progression. Patients received a median number of 5,5 cycles of therapy (range 1–24). We evaluated overall improvement (CR + PR+ HI), the best response obtained and adverse events in the overall study population, according to International Working Group MDS and LMA criteria. In the subgroup of patients who received at least 6 cycles of therapy (10 patients) we also evaluated overall survival (OS) and progression free survival (PFS).
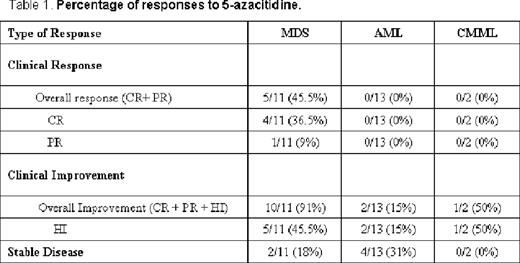
The results of 5-azacitidine therapy in our cohort of patients are described in Table 1.
In the AML cohort, after a median number of 4 cycles (range 1–10), we observed a hematological improvement (HI) in 15% of the patients, a stable disease (SD) in 31% of patients and a lack of response in 38% of patients. In the MDS cohort, after a median number of 7 cycles (range 2–24), we observed a complete response (CR) (including a cytogenetic response) in 36.5% of patients, a partial response (PR) in 9% of patients, a hematological improvement in 45.5% of patients and a stable disease in 18% of patients. The overall improvement (CR + PR + HI) was 15% in the AML cohort and 91% in the MDS cohort. In the LMMC cohort, after a median number of 2.5 cycles (range 1–4), we observed a hematological improvement in 50% of the patients.
In the subgroup of patients who received at least six cycles of therapy, the overall survival was 11.5 months and the progression free survival was 9 months. In the overall study population, two patients (8%) discontinued treatment as a result of adverse events. In four non-responder patients (15%) death was due to a rapid progression of disease.
In this analysis we have reported good response rates in MDS patients, with 36.5% of complete response (including a complete cytogenetic response). No CR or PR were observed in AML patients; however, in this subgroup of patients the median follow-up was short (median number of cycles of therapy: four). Furthermore, in these patients even a stable disease with no need of hospitalization and a good quality of life can be considered an important result. Due to the short period of follow-up, 57.5% of our patients received fewer than 6 cycles of 5-azacitidine and their therapy is still ongoing.
The limited number of cases and the short period of follow-up did not allow us to evaluate overall survival and progression free survival in the overall study population. We will update these data as time progresses. We reported these data in the subgroup of patients who received at least six cycles of therapy. According to current evidence, we observed that 5-azacitidine plays an important role in the treatment of patients with MDS (both with high- and low-IPSS risk) and low bone marrow blast counts AML. In these subgroups of patients, 5-azacitidine prolongs survival and is well tolerated. In our limited experience, this drug had no efficacy when a higher degree of bone marrow blasts (> 30%) was present.
Further trials should assess the number of cycles required for treatment, the role of hypometilating agents in low-risk MDS and in patients with AML and a bone marrow blasts counts > 30%.
No relevant conflict of interest to declare.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.