Abstract
Abstract 727
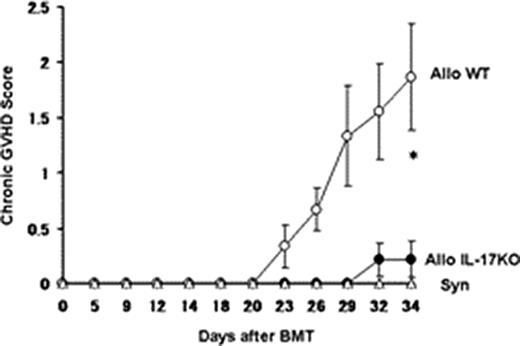
Chronic graft-versus-host disease (cGVHD) remains a major cause of late death and morbidity after allogeneic hematopoietic cell transplantation, and the treatment of cGVHD remains challenging. All-trans retinoic acid (ATRA), a potent derivative of vitamin A, can regulate immune responses. Am80, which has biological activity approximately 10 times more potent than that of ATRA by binding to RARα and RARβ, but not RARγ, also reduces the severity and progression of immune disease models, including contact dermatitis, collagen-induced arthritis, allergic encephalomyelitis, and atherosclerosis models. Am80 has been reported to suppress the differentiation of Th17 and Th1 cells. Previously, we demonstrated that the administration of ATRA or Am80, significantly decreased skin fibrosis and alopecia, a dominant feature of cutaneous cGVHD, using a well-characterized experimental model of cGVHD: B10.D2 (H−2d) → BALB/c (H−2d). Flow cytometry analysis of the peripheral lymph nodes (PLNs) on day 16 showed significant reductions in Th1, Th17, and Foxp3+ regulatory T cells (Tregs) in Am80-treated recipients, as compared to controls, whereas no reduction in Th2 cells was observed (Nishimori et al., 2009 ASH). To further investigate the roles of Th17 cells and other Th subsets (Th1 and Th2) in cGVHD, we first assessed the kinetics of Th cytokines in the B10.D2 (H-2d) → BALB/c (H-2d) model of cGVHD, which reflects the clinical and pathological symptoms of human cGVHD. BALB/c mice were subjected to sublethal irradiation (6.75 Gy) and injected with 8 × 106 T-cell-depleted bone marrow cells and 8 × 106 spleen cells or 2 × 106 CD90+ spleen T cells from B10.D2 mice. In the early phase (day 14) of post bone marrow transplant (BMT), donor T cells produced significantly less IL-17 in the PLNs of recipients in allogeneic BMT than in syngeneic BMT (1.68±0.09% vs. 4.30±0.53%, p<0.01), while in the late phase (day 28) donor T cells that produced IL-17 were increased significantly in allogeneic recipients, compared with syngeneic controls (7.76±0.27% vs. 1.61±0.16%, p < 0.005). Both IL-17−/IFN-γ+ and IL-17/IFN-γ double positive cells (Th17/Th1 cells) were constantly detected more frequently in allogeneic recipients (p<0.05). Next, we evaluated whether Th17 contributes in a model utilizing IL-17-deficient mice on a B10.D2 background as donor mice; these mice were backcrossed for more than six generations from the original knock-out (KO) mice. Upon transfer of IL-17−/− B10.D2 donor T cells in allogeneic BMT models, skin cGVHD was significantly ameliorated, as compared to recipients of wild-type (WT) T cells, as shown in Figure (p=0.02). Histopathological examination of the skin showed significantly reduced cGVHD pathology in recipients of IL-17−/− donors (3.17±1.09 vs. 8.50±0.84, p=0.006). Flow cytometry analysis of the PLNs, mesenteric lymph nodes (MLNs), and spleen cells in the early phase (day 14) showed no differences in Th1, Th2, and Tregs, while recipients of IL-17−/− had significantly fewer Th1 (p<0.05) and Th17/Th1 (p<0.01) cells on day 35. Furthermore, IFN-γ deficient mice on a B10.D2 background were also backcrossed from the original KO mice and cGVHD was evaluated. BMT from IFN-γ−/− donors significantly improved the clinical cGVHD score, compared with WT donors (p<0.05). Allogeneic recipients given anti-IFN-γ mAb (500 μg/mouse) on days 0, 5, 10, and 15 post BMT had significantly less severe cGVHD, compared with control antibody recipients (p<0.05). Taken together, Th17, especially in the late-chronic phase, and Th1 contribute to the development of cGVHD by promoting the production of proinflammatory cytokines. Targeting Th17 and Th1 may be a promising strategy for preventing and treating cGVHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.