Since then, almost no progress has been made in treating the virus that causes these tumors. In this issue of Blood, for the first time, Uldrick et al describe a long overdue approach to MCD therapy based on direct targeting of KSHV.4
There are now 7 known human cancer viruses but only scattered efforts to developed drugs specifically targeting them. The successes of the human papillomavirus and hepatitis B virus vaccines make clear that virus-oriented therapies have the potential to be major success stories in cancer management. If a virus causes a tumor, why are most pharmaceuticals targeting the host cancer cell instead of the causative virus? The most important reason is economics: 1 in 5 cancers worldwide has an infectious origin, with most cases concentrated in poor and developing countries.
But to be fair to the pharmaceutical industry, drugs against viral cancers are also difficult to make. Almost all current antivirals target viral replication machinery. The most well-known antiviral drug is acyclovir, a nucleoside analog activated by the herpes simplex thymidine kinase enzyme. This viral protein is only expressed during active viral replication to replicate viral DNA and for this reason acyclovir is effective against cold sores but not against latent virus in trigeminal or sacral ganglia. Acyclovir reduces symptoms but does not cure the underlying disease.
Similarly, viruses in most tumor cells are latent as well. If viruses in cancer cells did actively replicate, host innate and adaptive immune responses would kill the cell before it could grow into a clinically apparent tumor, and for most viral cancers there is no target that can be hit with available drugs. Ganciclovir, for example, is remarkably effective in randomized clinical trials to prevent KSHV replication and KS5,6 but has no effect once KS tumors emerge.7
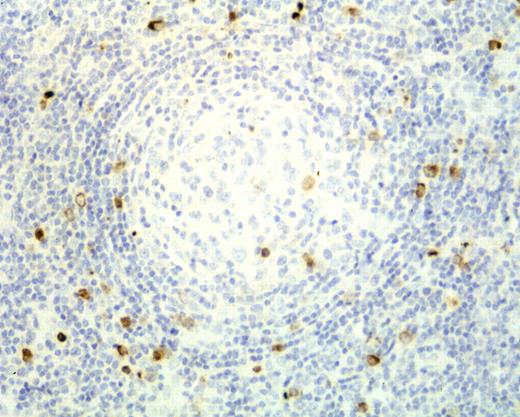
The study by Uldrick et al looks at this problem in a different way—are there any other KSHV-related tumors in which actively replicating virus can be targeted? Castleman disease is a B-cell lymphoproliferative disorder driven by IL-6 over-expression and in KSHV-related MCD, only a small percentage of tumor cells are actually KSHV-infected (see figure). KSHV-infected MCD cells are surrounded by uninfected B cells forced to multiply by cytokine-induced mitogenesis, which make up the bulk of MCD tumors and are responsible for most MCD symptoms and sequelae. Viral replication machinery plays a key role in MCD because KSHV-encoded vIL-6 is amplified as part of the virus's replication program (although the KSHV vIL-6 gene can be activated in different ways and should not be called a “lytic KSHV gene”).
KSHV-infected cells expressing vIL-6 within an adventitious germinal center in a multicentric Castleman disease tumor. Illustration courtesy of C. Parravicini.
KSHV-infected cells expressing vIL-6 within an adventitious germinal center in a multicentric Castleman disease tumor. Illustration courtesy of C. Parravicini.
Uldrick et al exploit this to develop a viral chemotherapy regimen against MCD. The work extends previous studies suggesting that antivirals can improve MCD patient survival.8 In their pilot study, Uldrick et al use the ganciclovir prodrug, valganciclovir, together with zidovudine (AZT) to precisely target 2 viral enzymes involved in viral DNA synthesis, the viral phosphotransferase and thymidine kinase, respectively—a first in KSHV oncology. These drugs can potentially be paired with other standard chemotherapies to further improve outcome for this disease that otherwise has a dismal prognosis.
Both drugs are approved for human use with other viral infections having more favorable pharmaco-economic indices than KSHV. In some African countries hard hit by AIDS, however, Kaposi sarcoma accounts for the majority of adult cancers reported to cancer registries. In Southeast Asia, EBV-containing nasopharyngeal carcinoma is a major unmet public health problem. Despite the effectivenesss of papillomavirus vaccines, cervical cancer remains a major killer throughout the developing world, and 4000 women die from it annually in the US. For KSHV and most other cancer viruses, the problem is not that there is no possible viral drug target. KSHV latency-associated nuclear antigen 1 is needed by the virus to maintain its genome in every tumor cell. Finding drugs to target these latent viral proteins is more an economic than a scientific issue. In the words of the astronaut Gus Grissom, “No bucks, no Buck Rogers.”
Rates of KS in developed countries have dramatically fallen with the development of effective antiretroviral therapy for HIV/AIDS, reducing the urgency to develop new control approaches to KSHV tumors. The current respite in KSHV-related disease, however, may be only temporary. Antiretroviral therapy does not affect latent, life-long KSHV infections and so resurgence of KSHV-related tumors with aging of the current HIV/AIDS population can be expected. We have not used this quiet time wisely.
This study by Uldrick et al provides a key lesson that antiviral chemotherapy in KSHV tumors can work—but only because of MCD's unusual pathoetiology. MCD acts more like a smoldering virus infection than a neoplasm. If new classes of antivirals were to be developed targeting latent cancer virus oncoproteins, there is promise that remarkable clinical outcomes could emerge. These drugs could lead to cures instead of palliation for some viral infections. They might also be far less toxic than current cancer chemotherapies because they target foreign proteins—much like the miraculous antibiotics of the 1940s. The study reported in this issue Blood is an important first step in this direction.
Conflict-of-interest disclosure: The authors hold patents related to KSHV that have been assigned to Columbia University. ■
REFERENCES
National Institutes of Health