Abstract
Endothelial urokinase-type plasminogen activator receptor (uPAR) is thought to provide a regulatory mechanism in angiogenesis. Here we studied the proangiogenic role of uPAR in endothelial colony-forming cells (ECFCs), a cell population identified in human umbilical blood that embodies all of the properties of an endothelial progenitor cell matched with a high proliferative rate. By using caveolae-disrupting agents and by caveolin-1 silencing, we have shown that the angiogenic properties of ECFCs depend on caveolae integrity and on the presence of full-length uPAR in such specialized membrane invaginations. Inhibition of uPAR expression by antisense oligonucleotides promoted caveolae disruption, suggesting that uPAR is an inducer of caveolae organization. Vascular endothelial growth factor (VEGF) promoted accumulation of uPAR in ECFC caveolae in its undegraded form. We also demonstrated that VEGF-dependent ERK phosphorylation required integrity of caveolae as well as caveolar uPAR expression. VEGF activity depends on inhibition of ECFC MMP12 production, which results in impairment of MMP12-dependent uPAR truncation. Further, MMP12 overexpression in ECFC inhibited vascularization in vitro and in vivo. Our data suggest that intratumor homing of ECFCs suitably engineered to overexpress MMP12 could have the chance to control uPAR-dependent activities required for tumor angiogenesis and malignant cells spreading.
Introduction
The term “angiogenesis ” connotes the process of new blood vessel formation from preexisting vessels.1,2 Identification of endothelial progenitor cells (EPCs) in peripheral blood has highlighted an alternative mechanism of vessel formation based on EPC recruitment from bone marrow.3 Similarly to endothelial cells (ECs), EPCs are able to migrate and differentiate to form primitive tubes in Matrigel. Moreover, EPCs can form endothelial-like colonies in vitro and show a high proliferative rate that is lacking in mature ECs.4
However, it is not yet clear how to define the EPCs that really contribute to vessel formation and their exact role in the process.5 In this study, we isolated cells from human umbilical cord blood (UCB), taking into consideration their capability to form a capillary network in vitro coupled with a high proliferation potential. Such a cell type was termed endothelial colony-forming cell (ECFC), as previously described.6-8
In the angiogenic process, ECs adhere to and degrade the extracellular matrix (ECM), proliferate, and differentiate into tubular-like structures.1,2,9 The membrane-associated plasminogen activation system (urokinase-type plasminogen activator [uPA]; uPA receptor [uPAR]; uPA inhibitor type-1 [PAI-1]) is critical in angiogenesis, being involved in uPA-mediated ECM degradation and uPAR-dependent cell adhesion.9 uPAR is a glycosylphosphatidylinositol-anchored protein that consists of 3 peptide domains (D1-D2-D3). It is present on the cell membrane as a full-length (D1+D2+D3) and a truncated molecule (D2+D3), unable to bind uPA, but retaining the property to interact with ECM molecules. We previously demonstrated that angiogenesis requires full-length uPAR. Indeed, in systemic sclerosis, a disease characterized by defective angiogenesis, the impairment of vessel formation is related also to overproduction of matrix metalloprotease-12 (MMP12), which truncates uPAR.10,11
The role of uPAR in ECFC-dependent vessel formation is less known. A single study indicated that EPCs display higher uPA activity and uPAR levels than mature ECs.12
Like other glycosylphosphatidylinositol-anchored molecules, uPAR is present in “lipid rafts,” dynamic microdomains of the cell membrane, rich in cholesterol, sphingolipids and glycolipids, trans-membrane protein receptors, integrins, and a large number of signaling molecules. However, uPAR can be found both in lipid rafts and nonraft fractions, and its distribution in different fractions is associated with different signaling pathways and, consequently, biologic processes.13,14 Caveolae are functionally and morphologically distinct forms of lipid rafts, characterized by the presence of the protein caveolin-1 and are particularly abundant in ECs, playing a fundamental role in their function.15 Vascular endothelial growth factor (VEGF) localizes in caveolae on interaction with its type 2 receptor, forming a “functional platform” involved in angiogenesis,16,17 together with other signaling molecules.
It is known that caveolae disruption affects biologic functions of the ECs, including angiogenesis.18 The aim of our study was to evaluate the relationship between caveolae and uPAR form/distribution on cell membrane in ECFC-dependent angiogenesis.
Here we show that ECFC angiogenesis depends on caveolae integrity and that uPAR induces caveolae formation. To assess the requirement of full-length uPAR in ECFC-dependent angiogenesis, we caused uPAR D1 truncation by transient transfection of MMP12, which resulted in inhibition of angiogenesis in vitro and in vivo.
Methods
Isolation and characterization of EPCs
Human UCB samples (volume > 50 mL) were collected in citrate phosphate dextrose solution from health newborns. We used cord blood units with a number of total nucleated cells < 1.3 × 109 (threshold of suitability for the banking established by the Umbilical Cord Bank of Careggi, Florence, Italy) after maternal informed consent in accordance with the Declaration of Helsinki and in compliance with Italian legislation.
EPCs have been isolated from UCB as previously described.4,7 Blood was diluted 1:1 with Hanks balanced salt solution (EuroClone) and was overlaid on an appropriate volume of density gradient separation medium (Lympholyte; Cedarlane). Cells were centrifuged for 30 minutes at room temperature at 740g. Mononuclear cells were recovered, washed 3 times with Hanks balanced salt solution and resuspended in complete EGM-2 medium (Lonza) supplemented with 10% FBS (Hyclone), 50 ng/mL VEGF (PeproTech) and 5 IU/mL heparin. Cells were seeded on gelatin-coated 6-well tissue culture plates at a density of 5 × 105 cells/cm2 in a 5% CO2 humidified incubator at 37°C. On days 4 and 7, half of the medium was exchanged with fresh medium. Then the medium was changed completely with EGM2–10% FBS every 3 days. EPC colonies appeared in cell cultures after 2-3 weeks and were identified as circumvented monolayers of cobblestone-like cells. These cells will be referred to as ECFCs, as previously described.7,19 The colonies were mechanically picked from the original plate and seeded on another gelatin-coated well with EGM2–10% FBS for expansion.
ECFCs were analyzed for the expression of surface antigens by flow cytometry. Washed cells were resuspended in flow cytometry buffer (CellWASH 0.1% sodium azide in PBS; BD Biosciences). Aliquots (0.1 × 106 cells/100 μL) were incubated with the following conjugated monoclonal antibodies: CD45-FITC, CD34-FITC, CD31-FITC (all from BD Biosciences PharMingen); CD105/R-phycoerythrin (Ancell); ULEX-FITC (Vector Laboratories); phycoerythrin-labeled by Tetra-Tag phycoerythrin-labeling kit (StemCell Technologies) KDR (RELIATech), uPAR/R3 (BioPorto Diagnostic A/S), and VWF (BD Biosciences PharMingen).
Nonspecific fluorescence and morphologic parameters of the cells were determined with isotype-matched mouse monoclonal antibodies (BD Biosciences PharMingen). All incubations were done for 20 minutes; and, after washing, cells were resuspended in 100 μL of CellWASH. 7-Amino-actinomycin (BD Biosciences PharMingen) was added to exclude dead cells from the analysis. Flow cytometric acquisition was performed by collecting 104 events on a FACSCalibur (BD Biosciences) instrument, and data were analyzed on DOT-PLOT biparametric diagrams using Cell Questpro OS X.1 software (BD Biosciences) on a Macintosh PC.
Caveolae isolation, characterization, modification, and silencing with siRNA
Isolation of ECFC caveolar raft and nonraft fractions was performed using a Caveolae/Rafts isolation kit (Sigma-Aldrich), based on separation on an OptiPrep density gradient, according to the manufacturer's instructions. After centrifugation (22 hours at 154 000g at 4°C), 9 fractions were collected. Caveolar raft and nonraft fractions were determined by Western blotting with anti–caveolin-1 antibodies (Sigma-Aldrich) for caveolar fractions. and anti-integrinβ1 antibodies (Santa Cruz Biotechnology) for nonraft fractions.20 To disrupt caveolae,21 we used methyl-β-cyclodextrin (β-MCD) (Sigma-Aldrich). Cholesterol depletion was measured as described.22 Cells were pretreated with 5mM β-MCD for 20 minutes at 37°C, and the cell extract was prepared at 4°C in lysis buffer containing 1% Triton X-100. Caveolin-1 silencing was performed by transfection of ECFCs with small interfering RNA (siRNA) and negative control constructs (Dharmacon RNA Technologies/Euroclone), according to the manufacturer's instructions.
Western blot and RT-PCR analysis
Cell lysates were obtained, processed, and blotted as described.10 The primary antibodies were: anti–caveolin-1 (1:1000; rabbit polyclonal antibody, Sigma-Aldrich); anti-uPAR R3 (1:500; mouse monoclonal antibody, BioPorto Diagnostics), which recognizes the full-length uPAR; anti-uPAR M2 (1 μg/mL, rabbit polyclonal antibody, provided by Dr D'Alessio, Istituto Humanitas), which reveals both the full-length and truncated form of uPAR; anti-MMP12 (1:500; rabbit polyclonal antibody; Chemicon International); phospho-ERK (p42/p44; 200 μg/mL, 1:500) and ERK-2 (200 μg/mL, 1:500; Santa Cruz Biotechnology). Aliquots of caveolar raft and nonraft fractions20 were subjected to Western blotting. After incubation with HRP-conjugated anti–rabbit IgG (1:5000) for 1 hour (GE Healthcare), immune complexes were detected with the enhanced chemiluminescence detection system (GE Healthcare). Membranes were exposed to autoradiographic films (Hyperfilm MP; GE Healthcare) for 1-30 minutes.
Treatments inducing uPAR up-regulation/inhibition
VEGF (50 ng/mL; Calbiochem-VWR International) was used to up-regulate uPAR in ECFCs. After overnight VEGF stimulation in EGM2-2% FCS, cells were recovered, and the supernatant was dialyzed against distilled water and lyophilized. To inhibit uPAR expression, we treated ECFCs with anti-uPAR aODNs in a complex with DOTAP (Boehringer Mannheim), as reported.23,24 As a negative control, we used a scrambled ODN. ECFCs were treated daily for 4 days; then the cells and the medium were recovered and used in in vitro studies. The term “control cells” refers to ECFCs cultivated in the presence of DOTAP, which does not affect cell viability.23
Immunofluorescence confocal microscopy
Control and treated ECFCs were grown on coverslips, fixed, and permeabilized according to routine methods.25 The anti–human primary antibodies used were: anti-uPAR R3 (1:40), anti-caveolin-1 (1:400). The secondary antibodies were: CY3-conjugated anti–mouse IgG (1:800; Sigma-Aldrich) and FITC-conjugated anti–rabbit IgG (1:800; Sigma-Aldrich). For nuclear staining, samples were incubated with 4,6-diamidino-2-phenylindole (2 μg/mL), for 15 minutes. In negative control slides primary antibody was omitted. Coverslips were mounted with antifade mounting medium (Biomeda) and imaged on a Bio-Rad MRC 1024 ES confocal laser scanning microscope (Bio-Rad) equipped for fluorescence measurements. Images were acquired by using Bio-Rad confocal EZ-C1 3.40 Gold Version software. Maximum intensity projections of the acquired image stacks were constructed, analyzed, and color-combined by using ImageJ 1.44 software (www.rsb.info.nih.gov/ij; National Institutes of Health), also used for statistical evaluation of caveolar cluster areas, uPAR/Cav-1 colocalization,26 fluorescence intensities, and background signals. Colocalization was determined through the “Just Another Colocalization Plugin”27 (JACoP) of ImageJ 1.44 software. Caveolae for each cell were obtained by isolating high fluorescent spots, restricting the fluorescent spot by size, and processing data with the “Analyze Particle” command contained in ImageJ 1.44 software.
In vitro parameters of angiogenesis
Invasion was studied in Boyden chambers using porous filters coated with Matrigel (50 μg/filter).10,24 ECFCs (20 × 103) were placed in the top compartment of the chamber and migration, evaluated after 6 hours, was expressed as the absolute number of migrated cells ± SD. Where detailed, ECFC invasion was stimulated by 50 ng/mL VEGF in the bottom chamber. In other experiments ECFCs were pretreated with 5mM β-MCD for 20 minutes at 37°C or subjected to caveolin-1 silencing. Some experiments were performed in the presence of anti-uPAR R3 antibody or irrelevant IgG (all used at 1.5 μg/ml) or after anti-uPAR aODN treatment. Capillary morphogenesis was performed in 13-mm tissue culture wells coated with Matrigel, as described.10,24 Experimental conditions were the same used for invasion assay. ECFCs were plated (60 × 103/well) in complete EBM-2 medium 2% FCS and incubated at 37°C, 5% CO2. Plates were photographed at 6 hours and at 24 hours. Results were quantified by image analysis, giving the percentage of photographic field occupied by ECFC. Six to 9 photographic fields from 3 plates were scanned for each point. Results were expressed as percentage field occupancy with respect to control taken as 100% ± SD.
MMP-12 transient transfection
ECFCs (1 × 107 cells) were incubated in 500 μL EBM-2 medium with the addition of recombinant vectors (15 μg each of either pCDNA3.1 + MMP12 or pCDNA3.1 alone; Invitrogen) and electroporated using a Gene Pulser apparatus (0.260 KV, 0.975 μF; Bio-Rad). Production of recombinant MMP12 vector and the expression of MMP12 gene and protein were previously described.11 Expression of MMP12 gene was measured by RT-PCR, and the level of released protein was analyzed by Western blotting of culture medium.
MMP-12–dependent uPAR cleavage
To verify MMP12-dependent uPAR cleavage, 25 μg of recombinant human uPAR (R&D Systems) was incubated overnight at 37°C with 15 μL of EBM2–2% FBS (control) or conditioned medium (CM) derived from empty vector or MMP-12 transiently transfected ECFCs. These experiments were performed in the absence and in the presence of anti-MMP12 antibody (10 μg/mL), which inhibits the MMP12 catalytic activity, as shown in Table 2. CMs were dialyzed against distilled water, lyophilized, and reconstituted (10×). After incubation, the samples were processed and subjected to Western blotting with anti-uPAR M2 antibody.
Matrigel-sponge assay in mice
Aliquots of 50 μL reconstituted CM from empty-vector, and MMP-12–transfected ECFCs, containing 50 U/mL heparin, were added to unpolymerized Matrigel at 4°C at a final volume of 0.6 mL, in the absence or in the presence of anti-MMP12 antibody (10 μg/mL). The Matrigel suspension was injected subcutaneously into the flanks of C57/BL6 male mice (Charles River) using a cold syringe (4 injections/animal). At body temperature, the Matrigel polymerizes to a solid gel, which becomes vascularized within 4 days in response to CM. Pellets were removed, photographed, minced, and diluted in water to measure the hemoglobin content with a Drabkin reagent kit (Sigma-Aldrich). To verify the enzymatic activity of MMP12 within the recovered Matrigel sponges, we solubilized the plugs,28 incubated aliquots of the solubilized plugs with standard uPAR and then evaluated uPAR truncation by Western blotting, using the M2 antibody. All mouse experiments were approved by the Italian Ministry of Health Animal Care and Use Committee.
Statistics
Results were expressed as mean ± SD of the indicated number of experiments. Multiple comparisons were performed by the Student-Newman-Keuls test, after demonstration of significant differences among medians by nonparametric variance analysis according to Kruskal-Wallis. Statistical significances were accepted at P < .05.
Results
Isolation and characterization of ECFCs
ECFCs have been isolated from the blood of 10 of 12 umbilical cords. ECFCs were considered as EPC-derived cells,7,19 which originated from adherent cell population after 14-21 days of culture. After 21 days, the median frequency of ECFCs was 0.12 colonies/106 mononuclear cells (range, 0.03-0.57). UCB-ECFCs used showed a high proliferative potential and could be expanded to at least P15 without signs of senescence. The mean proliferation index was 10.7 (SD = 6.1) at P2, 10.2 at P5 (SD = 6.8), and 10.1 at P10 (SD = 6.7). Immunophenotyping by FACS analysis revealed that CB ECFCs expressed endothelial cell surface antigens CD31, ULEX, and CD105. Low levels of KDR and VWF were detected. In addition, uPAR was revealed (Table 3), whereas CD45 and CD34 were almost undetectable. In vitro morphology (Figure 1A left panel) and capillary morphogenesis (Figure 1A central and right panels) of ECFCs resembled that of mature ECs.
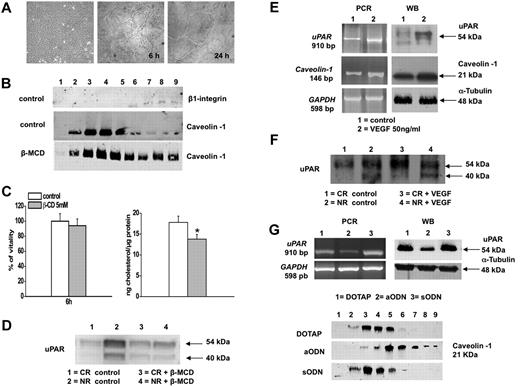
Relationship between caveolae and uPAR distribution in ECFC cell membrane. (A) Morphologic profile of ECFC colonies appeared after 2–3 weeks of culture (left panel). Capillary-morphogenesis in vitro at 6 and 24 hours (middle and right panel); (B) Caveolin-1 distribution. Cell lysates were layered on Optiprep solution and centrifuged as described in “Methods” to separate lipid rafts (fractions 2-6) from (fractions 7-9) in control conditions and after treatment with β-MCD (5mM for 20 minutes). Fractions obtained were probed by Western blotting with specific anti–caveolin-1 and anti-integrin β1 antibodies, as caveolar raft and nonraft marker respectively. Data are representative of 5 independent experiments. (C) β-MCD-treatment: right panel shows the β-MCD-induced cholesterol depletion. Evaluation of cholesterol amount was performed as previously described22 ; left panel shows vitality of the β-MCD-treated cells determined by trypan blue dye exclusion test. *P < .05, significantly different from control; (D) uPAR distribution: control and β-MCD–treated cells were subjected to Optiprep gradient separation and caveolar raft (CR) and nonraft (NR) fractions were analyzed by Western blotting with anti-uPAR antibody M2, which reveals both the full length and truncated uPAR. Numbers on the right indicates molecular weights expressed in kilodaltons. Data are representative of 5 independent experiments performed with clones expressing different levels of uPAR; (E) VEGF treatment: expression of uPAR and caveolin-1. Left panels: PCR of uPAR and caveolin-1 cDNA in untreated (control; lane 1) and VEGF-treated (lane 2) ECFCs. Numbers on the left indicate the size of PCR products in base pairs (bp). GAPDH: glyceraldehyde-3-phosphate dehydrogenase used as housekeeping gene. Right panels show Western blotting for uPAR and caveolin-1. Numbers on the right indicate molecular weights expressed in kilodaltons; (F) uPAR distribution in control and in VEGF-treated ECFCs. Control and VEGF-treated cells were subjected to Optiprep gradient separation: caveolar raft (CR) and nonraft (NR) fractions were collected and analyzed by Western blotting with anti-uPAR antibody M2. Numbers on the right indicate molecular weights expressed in kilodaltons; (G) silencing of uPAR gene using anti-uPAR aODNs: cell cultures were treated with aODN for 4 days in the presence of the cationic phospholipid DOTAP. A scrambled ODN (sODN) was used as a negative control. Top panels: PCR of ODNs-treated cells (on the left); Western blotting of ODNs-treated cells (α-tubulin was used as a loading control; on the right). Bottom panels: distribution of caveolin in Optiprep-prepared caveolar rafts after ODNs treatment. Data shown in panels E, F, and G are representative of 5 independent experiments.
Relationship between caveolae and uPAR distribution in ECFC cell membrane. (A) Morphologic profile of ECFC colonies appeared after 2–3 weeks of culture (left panel). Capillary-morphogenesis in vitro at 6 and 24 hours (middle and right panel); (B) Caveolin-1 distribution. Cell lysates were layered on Optiprep solution and centrifuged as described in “Methods” to separate lipid rafts (fractions 2-6) from (fractions 7-9) in control conditions and after treatment with β-MCD (5mM for 20 minutes). Fractions obtained were probed by Western blotting with specific anti–caveolin-1 and anti-integrin β1 antibodies, as caveolar raft and nonraft marker respectively. Data are representative of 5 independent experiments. (C) β-MCD-treatment: right panel shows the β-MCD-induced cholesterol depletion. Evaluation of cholesterol amount was performed as previously described22 ; left panel shows vitality of the β-MCD-treated cells determined by trypan blue dye exclusion test. *P < .05, significantly different from control; (D) uPAR distribution: control and β-MCD–treated cells were subjected to Optiprep gradient separation and caveolar raft (CR) and nonraft (NR) fractions were analyzed by Western blotting with anti-uPAR antibody M2, which reveals both the full length and truncated uPAR. Numbers on the right indicates molecular weights expressed in kilodaltons. Data are representative of 5 independent experiments performed with clones expressing different levels of uPAR; (E) VEGF treatment: expression of uPAR and caveolin-1. Left panels: PCR of uPAR and caveolin-1 cDNA in untreated (control; lane 1) and VEGF-treated (lane 2) ECFCs. Numbers on the left indicate the size of PCR products in base pairs (bp). GAPDH: glyceraldehyde-3-phosphate dehydrogenase used as housekeeping gene. Right panels show Western blotting for uPAR and caveolin-1. Numbers on the right indicate molecular weights expressed in kilodaltons; (F) uPAR distribution in control and in VEGF-treated ECFCs. Control and VEGF-treated cells were subjected to Optiprep gradient separation: caveolar raft (CR) and nonraft (NR) fractions were collected and analyzed by Western blotting with anti-uPAR antibody M2. Numbers on the right indicate molecular weights expressed in kilodaltons; (G) silencing of uPAR gene using anti-uPAR aODNs: cell cultures were treated with aODN for 4 days in the presence of the cationic phospholipid DOTAP. A scrambled ODN (sODN) was used as a negative control. Top panels: PCR of ODNs-treated cells (on the left); Western blotting of ODNs-treated cells (α-tubulin was used as a loading control; on the right). Bottom panels: distribution of caveolin in Optiprep-prepared caveolar rafts after ODNs treatment. Data shown in panels E, F, and G are representative of 5 independent experiments.
Caveolae and uPAR distribution on cell membrane
ECFC extracts were subjected to density-gradient separation. Fractions were assayed by Western blotting for the presence of caveolin-1, as caveolar marker (2-6) and of integrin-β1 as nonraft marker (7-9, Figure 1B top and middle panels). Many studies propose an important role of intact caveolae in the regulation of angiogenesis.29,30 Among the methods available to modify the membrane raft composition,21 here we used β-MCD, which induces cholesterol depletion (Figure 1C right panel). Because β-MCD could be toxic for the cells, we first checked for the experimental nontoxic conditions together with the caveolar raft disruption, evaluating ECFC vitality by morphology and trypan blue exclusion. After treatment with 5mM β-MCD for 20 minutes, the cells were still viable (Figure 1C left panel) and showed a normal morphology (data not shown), and caveolin-1 was distributed in all the fractions, thus demonstrating the disruption of normal lipid organization (Figure 1B bottom panel). In control conditions, uPAR was mainly present in nonraft fractions, whereas it redistributed in caveolar and nonraft fractions on β-MCD (Figure 1D). VEGF treatment up-regulated both caveolin-1 and uPAR (Figure 1E). A large amount of uPAR shifted from nonraft to the caveolar fraction after VEGF treatment (Figure 1F), and mainly the full-length uPAR was present in caveolae, whereas the truncated form was restricted to nonraft fractions, indicating that VEGF also affects the membrane distribution of full-length uPAR on ECFCs. These results are representative of independent experiments in ECFC clones expressing different uPAR levels.
The parallel increase of uPAR and caveolin-1 led us to hypothesize a potential role of uPAR in caveolae formation. To corroborate our hypothesis, we inhibited uPAR expression by anti-uPAR aODNs (Figure 1G), which resulted in a decrease of uPAR mRNA and protein (top panels). This treatment also caused redistribution of caveolin-1 from caveolar rafts to all the fractions (bottom panels), similarly to β-MCD, thus demonstrating a loss of native lipid organization on cell surface in the absence of uPAR.
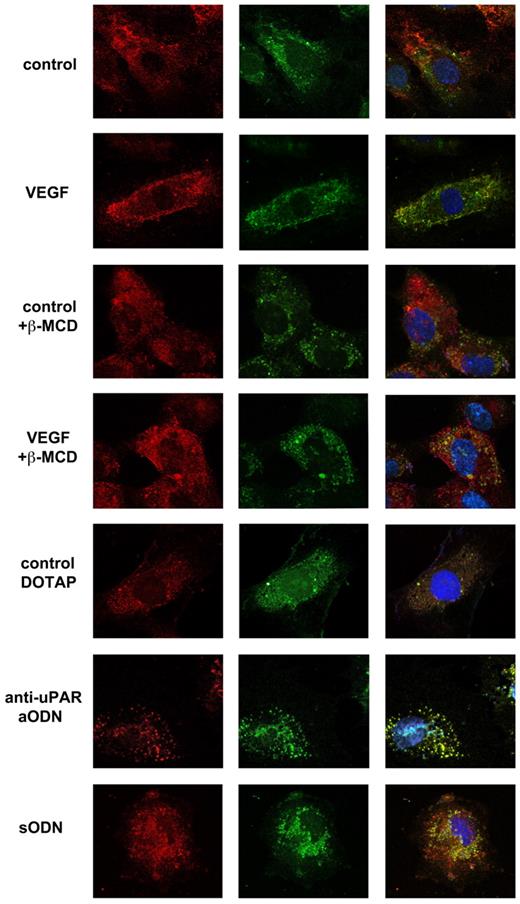
Immunofluorescence analysis: colocalization uPAR/caveolin-1
Because uPAR was found in caveolar rafts, we tested uPAR-caveolin colocalization by immunofluorescence in all our experimental conditions. Figure 2 shows that untreated ECFCs had a homogeneous dotted distribution of uPAR and a partial colocalization of uPAR with caveolin-1, whereas VEGF treatment induced an increase of fluorescence intensity of both caveolin-1 and uPAR together with a more strong evidence of colocalization. Caveolar rafts disruption by β-MCD led to a loss of caveolin-1/uPAR colocalization, only partially recovered in VEGF-treated cells. Inhibition of uPAR expression by anti-uPAR aODN caused the loss of uPAR fluorescence signal but not of colocalization. Scrambled ODN-treated cells maintained fluorescence levels and colocalization as in control cells.
Colocalization uPAR/caveolin-1 and caveolar rafts analysis by immunofluorescence. Immunostaining of uPAR and caveolin-1 in ECFCs in different experimental conditions. Panels on the left represent uPAR staining (red represents Cy3) using anti-uPAR R3 antibody, which identifies full-length uPAR; central panels correspond to caveolin-1 staining (green represents FITC), using anti-caveolin-1 antibody and right panels show the double staining of ECFCs with anti-uPAR (red) and anti–caveolin-1 (green). Nuclear staining is obtained by the use of 4,6-diamidino-2-phenylindole (blue). Cells were observed with an inverted confocal Nikon Eclipse TE2000 microscope equipped with a Nikon S Fluor 60× oil immersion lens (Nikon). Images were acquired at room temperature, using a standard 1024- by 1024-pixel image format and adjusting the zoom level to match the voxel size to the Nyquist criterion. The pinhole size was always set at 1 airy unit (airy disk), and each plane was Kalman averaged to reduce noise. In each experiment, the same instrumental settings were used for all image acquisitions. All images were Gaussian filtered to eliminate single-pixel noise before analysis (original magnification × 600).
Colocalization uPAR/caveolin-1 and caveolar rafts analysis by immunofluorescence. Immunostaining of uPAR and caveolin-1 in ECFCs in different experimental conditions. Panels on the left represent uPAR staining (red represents Cy3) using anti-uPAR R3 antibody, which identifies full-length uPAR; central panels correspond to caveolin-1 staining (green represents FITC), using anti-caveolin-1 antibody and right panels show the double staining of ECFCs with anti-uPAR (red) and anti–caveolin-1 (green). Nuclear staining is obtained by the use of 4,6-diamidino-2-phenylindole (blue). Cells were observed with an inverted confocal Nikon Eclipse TE2000 microscope equipped with a Nikon S Fluor 60× oil immersion lens (Nikon). Images were acquired at room temperature, using a standard 1024- by 1024-pixel image format and adjusting the zoom level to match the voxel size to the Nyquist criterion. The pinhole size was always set at 1 airy unit (airy disk), and each plane was Kalman averaged to reduce noise. In each experiment, the same instrumental settings were used for all image acquisitions. All images were Gaussian filtered to eliminate single-pixel noise before analysis (original magnification × 600).
To estimate the caveolar cluster number/size and colocalization ratio between caveolin-1 and uPAR, we performed the fluorescence analysis. As shown in Table 4, VEGF treatment increased caveolar cluster number and size, as well as uPAR/caveolin1 colocalization compared with control. The β-MCD treatment caused a decrease of number and size of caveolar clusters and a reduction of uPAR/caveolin-1 colocalization, only partially recovered after VEGF treatment. uPAR silencing by aODNs resulted in a drastic decrease of number and size of caveolar clusters.
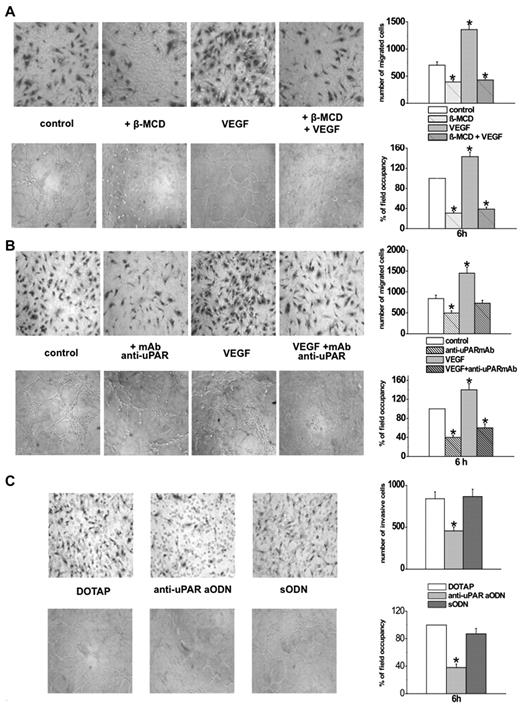
Role of caveolae and uPAR in in vitro ECFC angiogenesis and VEGF signaling
To evaluate the role of caveolae in ECFC-dependent angiogenesis in vitro, we performed Matrigel invasion and capillary morphogenesis after β-MCD treatment and caveolin-1 silencing. β-MCD treatment impaired basal and VEGF-stimulated ECFC invasion (Figure 3A top panels) and capillary morphogenesis (Figure 3A bottom panels). In some experiments, we added β-MCD for 20 minutes to preorganized capillary-like networks and observed the loss of preexistent capillary tubular structure (not shown).
Role of caveolae and uPAR in in vitro ECFC-dependent angiogenesis. In vitro angiogenesis was measured by Matrigel invasion and by capillary morphogenesis of ECFCs after modification of caveolar rafts or of uPAR expression. In all the experiments, results are the mean of 3 different experiments performed in triplicate in 3 different ECFC preparations. The histograms on the right of each panel refer to the relative quantification and are expressed as mean value ± SD. *P < .05, significantly different from control. In all the histograms, Matrigel invasion is expressed as the absolute number of migrated cells, by directly counting the migrated cells on the filters, whereas capillary morphogenesis is quantified by measuring the percentage field occupancy of capillary projections, assuming the control as 100%. Six to 9 photographic fields from 3 plates were scanned for each point. (A) Effects of caveolar raft modification. Top part: Matrigel invasion of ECFCs before and after treatment with 5mM β-MCD, in control and after VEGF stimulation (50 ng/mL). Bottom part: Capillary morphogenesis at 6 hours in the same conditions (symbols as in Figure 1). (B) The experimental conditions were the same as in panel A, but cells were treated with anti-uPAR antibodies (antibody R3) instead of β-MCD. Top panels: Matrigel invasion. Bottom panels: Capillary morphogenesis under the same experimental conditions. (C) Silencing of uPAR gene using the anti-uPAR aODN. Top panels: Matrigel invasion of control (DOTAP) untreated and 4 days ODN-treated ECFCs in the presence of DOTAP. The same experimental conditions were used for capillary morphogenesis (bottom panels).
Role of caveolae and uPAR in in vitro ECFC-dependent angiogenesis. In vitro angiogenesis was measured by Matrigel invasion and by capillary morphogenesis of ECFCs after modification of caveolar rafts or of uPAR expression. In all the experiments, results are the mean of 3 different experiments performed in triplicate in 3 different ECFC preparations. The histograms on the right of each panel refer to the relative quantification and are expressed as mean value ± SD. *P < .05, significantly different from control. In all the histograms, Matrigel invasion is expressed as the absolute number of migrated cells, by directly counting the migrated cells on the filters, whereas capillary morphogenesis is quantified by measuring the percentage field occupancy of capillary projections, assuming the control as 100%. Six to 9 photographic fields from 3 plates were scanned for each point. (A) Effects of caveolar raft modification. Top part: Matrigel invasion of ECFCs before and after treatment with 5mM β-MCD, in control and after VEGF stimulation (50 ng/mL). Bottom part: Capillary morphogenesis at 6 hours in the same conditions (symbols as in Figure 1). (B) The experimental conditions were the same as in panel A, but cells were treated with anti-uPAR antibodies (antibody R3) instead of β-MCD. Top panels: Matrigel invasion. Bottom panels: Capillary morphogenesis under the same experimental conditions. (C) Silencing of uPAR gene using the anti-uPAR aODN. Top panels: Matrigel invasion of control (DOTAP) untreated and 4 days ODN-treated ECFCs in the presence of DOTAP. The same experimental conditions were used for capillary morphogenesis (bottom panels).
On the basis of uPAR involvement in angiogenesis31,32 and of our data showing its role in caveolae formation (Figures 1G and 2), we evaluated the function of caveolar uPAR in ECFC-dependent angiogenesis by uPAR up-regulation or uPAR inhibition. To increase uPAR, we stimulated ECFCs with VEGF (Figure 1E) in the absence or in the presence of monoclonal anti-uPAR-R3. As shown in Figure 3B, R3 reduced ECFC Matrigel invasion and capillary morphogenesis in basal conditions, as well as their VEGF-dependent increase, thus demonstrating that the proangiogenic role of VEGF involves uPAR up-regulation.
We silenced uPAR gene using anti-uPAR aODNs, shown here to abolish uPAR expression and caveolae formation (Figure 1G). Figure 3C shows that aODN treatment specifically impaired ECFC invasion and capillary morphogenesis.
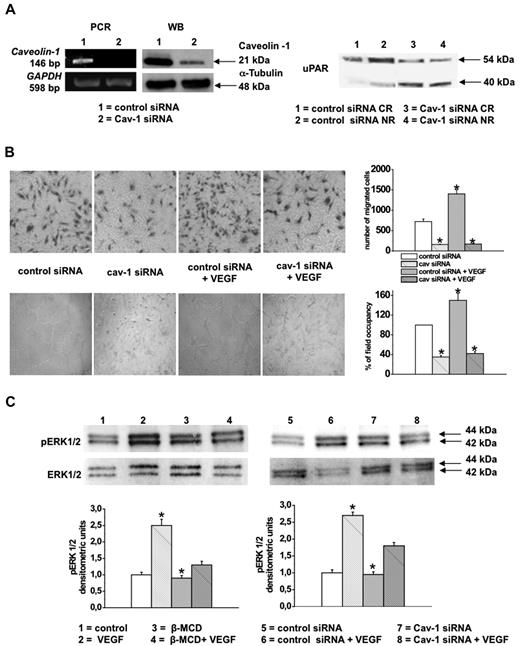
On caveolin-1 silencing (Figure 4A left), full-length and truncated uPAR redistribution was similar to that obtained after β-MCD treatment (Figure 4A right). In addition, ECFC invasion and capillary morphogenesis in basal conditions and after VEGF stimulation were impaired (Figure 4B).
Caveolin-1 silencing. Effects on invasion, capillary morphogenesis and VEGF signaling. (A) Left panels: PCR and Western blotting of caveolin-1 silencing in ECFCs. Numbers on the left: size of PCR products (bp); numbers on the right: molecular weights expressed in kilodaltons. Right panel: Western blotting of uPAR distribution between caveolar raft (CR) and nonraft (NR) fractions under control conditions (scrambled-sequence siRNA) and after caveolin-1 silencing (Cav-1 siRNA). uPAR was revealed with M2 antibody. Numbers on the right: molecular weights expressed in kilodaltons. Results were similar to those Figure 1D, obtained with β-MCD. (B) Effects of caveolin-1 silencing on basal and VEGF-stimulated ECFC Matrigel invasion (top panels) and ECFC capillary morphogenesis (bottom panels). For image acquisition and quantification, refer to the legends of Figures 1 and 3. Quantification is shown by histograms on the right: values refer to 3 experiments performed in triplicate in 3 different ECFC cell lines. Data are expressed as mean value ± SD. *P < .05, significantly different from control. (C) Western blotting with anti-pERK1/2 antibodies in the experimental conditions reported in the bottom captions (control conditions, β-MCD treatment, caveolin-1 silencing, and VEGF stimulation), showing that both β-MCD treatment and caveolin-1 silencing inhibited VEGF-dependent ERK1/2 phosphorylation. ERK1/2 indicates loading control obtained with anti-total ERK1/2 antibodies. Numbers on the right: molecular weight expressed in kilodaltons. Histograms on the bottom show quantification of Western blotting experiments (as densitometric units) and refer to 3 experiments performed in triplicate in 3 different ECFC lines. Data are expressed as mean value ± SD. *P < .05, significantly different from control.
Caveolin-1 silencing. Effects on invasion, capillary morphogenesis and VEGF signaling. (A) Left panels: PCR and Western blotting of caveolin-1 silencing in ECFCs. Numbers on the left: size of PCR products (bp); numbers on the right: molecular weights expressed in kilodaltons. Right panel: Western blotting of uPAR distribution between caveolar raft (CR) and nonraft (NR) fractions under control conditions (scrambled-sequence siRNA) and after caveolin-1 silencing (Cav-1 siRNA). uPAR was revealed with M2 antibody. Numbers on the right: molecular weights expressed in kilodaltons. Results were similar to those Figure 1D, obtained with β-MCD. (B) Effects of caveolin-1 silencing on basal and VEGF-stimulated ECFC Matrigel invasion (top panels) and ECFC capillary morphogenesis (bottom panels). For image acquisition and quantification, refer to the legends of Figures 1 and 3. Quantification is shown by histograms on the right: values refer to 3 experiments performed in triplicate in 3 different ECFC cell lines. Data are expressed as mean value ± SD. *P < .05, significantly different from control. (C) Western blotting with anti-pERK1/2 antibodies in the experimental conditions reported in the bottom captions (control conditions, β-MCD treatment, caveolin-1 silencing, and VEGF stimulation), showing that both β-MCD treatment and caveolin-1 silencing inhibited VEGF-dependent ERK1/2 phosphorylation. ERK1/2 indicates loading control obtained with anti-total ERK1/2 antibodies. Numbers on the right: molecular weight expressed in kilodaltons. Histograms on the bottom show quantification of Western blotting experiments (as densitometric units) and refer to 3 experiments performed in triplicate in 3 different ECFC lines. Data are expressed as mean value ± SD. *P < .05, significantly different from control.
We next investigated the effect of caveolae disruption on VEGF-induced signaling. We observed that VEGF stimulated ERK1/2 phosphorylation in ECFC, whereas β-MCD treatment and caveolin-1 silencing markedly reduced VEGF-induced ERK1/2 activation (Figure 4C). These results demonstrated the requirement of caveolar rafts integrity on VEGF signaling in ECFCs.
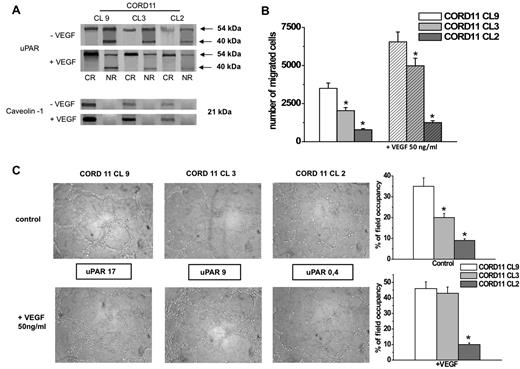
A correlation between uPAR expression/distribution and angiogenesis in control and VEGF-challenged ECFC was investigated. Clones expressing different uPAR levels were subjected to Western blotting to assess uPAR distribution with M2 antibody in caveolar raft and nonraft fractions. On VEGF, full-length uPAR was mainly present in the caveolar fraction (Figure 5A), whereas the truncated form was selectively present in nonraft fraction. ECFC clones expressing higher levels of uPAR were more prone to invade Matrigel as well as to form capillary-like tubes in vitro (Figure 5B and C, respectively). In addition, the response to the VEGF was dependent on uPAR levels. In addition, we determined caveolin-1 expression in the 3 different clones of Figure 4A, finding a positive correlation between uPAR and caveolin-1 expression, providing further support to a functional link between uPAR expression and caveolae organization.
Relationship between uPAR levels and in vitro angiogenesis. (A) Different clones, displaying different levels and distribution of uPAR, evaluated by Western blotting analysis for uPAR and caveolin-1 expression in basal conditions (−VEGF) and after VEGF challenge (+VEGF). Numbers on the right indicate molecular weight. The pictures show the results of a typical experiment of 3 that gave similar results. (B) Matrigel invasion of different ECFC clones in control conditions and in VEGF-stimulated cells. The histograms refer to quantification, expressed as number of migrated cells, of 3 different experiments performed in triplicate with each clone. Results are shown as mean value ± SD. *P < .05, significantly different from control. (C) In vitro capillary morphogenesis of different ECFC clones displaying different uPAR levels. The numbers in the frame represent the percentage of uPAR-positive cells. Histograms on the right show quantification of capillary morphogenesis experiments (under control conditions an VEGF stimulation, respectively). Image acquisition and quantification were performed as reported in Figures 1 and 3. Results are representative of a typical experiment of 3 experiments performed in triplicate with each clone and are quantified by measuring the absolute percentage field occupancy of capillary projections. *P < .05, significantly different from control.
Relationship between uPAR levels and in vitro angiogenesis. (A) Different clones, displaying different levels and distribution of uPAR, evaluated by Western blotting analysis for uPAR and caveolin-1 expression in basal conditions (−VEGF) and after VEGF challenge (+VEGF). Numbers on the right indicate molecular weight. The pictures show the results of a typical experiment of 3 that gave similar results. (B) Matrigel invasion of different ECFC clones in control conditions and in VEGF-stimulated cells. The histograms refer to quantification, expressed as number of migrated cells, of 3 different experiments performed in triplicate with each clone. Results are shown as mean value ± SD. *P < .05, significantly different from control. (C) In vitro capillary morphogenesis of different ECFC clones displaying different uPAR levels. The numbers in the frame represent the percentage of uPAR-positive cells. Histograms on the right show quantification of capillary morphogenesis experiments (under control conditions an VEGF stimulation, respectively). Image acquisition and quantification were performed as reported in Figures 1 and 3. Results are representative of a typical experiment of 3 experiments performed in triplicate with each clone and are quantified by measuring the absolute percentage field occupancy of capillary projections. *P < .05, significantly different from control.
Full-length uPAR is required to perform angiogenesis in vitro and in vivo
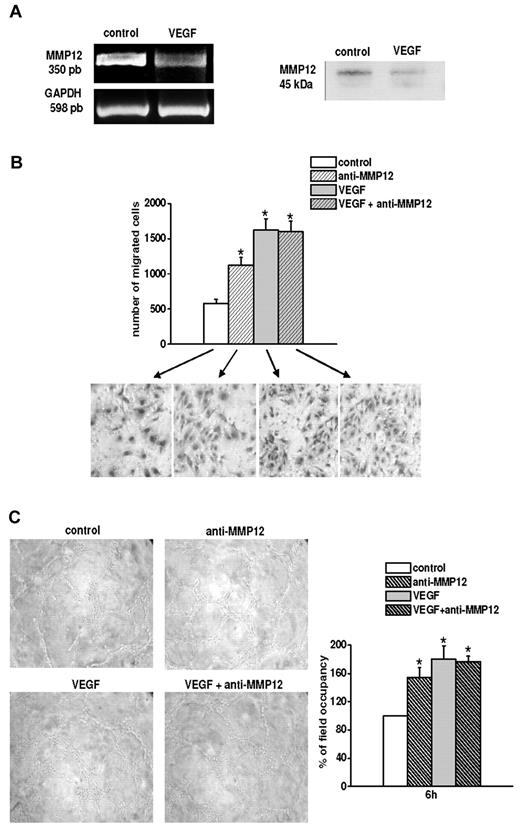
The data shown in Figure 1 demonstrate that VEGF up-regulates uPAR and recruits its full-length form into caveolae, thus increasing angiogenesis in vitro (Figure 3). We have previously shown that MMP12 uPAR D1 cleavage results in angiogenesis impairment.10 Thus, we investigated whether VEGF treatment of ECFCs also decreased MMP12 synthesis and consequently uPAR truncation, which could be in agreement with the increased angiogenic properties of VEGF-treated ECFCs. Figure 6A shows PCR and Western blotting analysis, indicating that VEGF-treated ECFCs expressed lower amounts of MMP12 than untreated cells.
In vitro MMP12-dependent angiogenesis. (A) Left panel: RT-PCR of MMP12 in control and VEGF-treated ECFCs. Right panel: Western blot analysis of MMP12 revealed in the culture medium of control and VEGF-treated ECFCs. (B) Matrigel invasion of control and VEGF-treated ECFCs, in the absence and in the presence of anti-MMP12 antibody (10 μg/mL), under basal conditions (control), and after VEGF stimulation. Histogram refers to quantification of Matrigel invasion assay obtained by counting the total number of migrated cells/filter. Results are the mean of 3 different experiments performed in triplicate in 3 ECFC preparations and are shown as mean value ± SD. *P < .05, significantly different from control. (C) Capillary morphogenesis of ECFCs using the same experimental conditions described for panel B. The figures are representative of a typical experiment of 3 experiments performed in triplicate in 3 ECFC preparations. Quantification was performed by measuring the percentage field occupancy of capillary projections, taking the control as 100%. *P < .05, significantly different from control. Image acquisition and quantification were performed as described in Figures 1 and 3.
In vitro MMP12-dependent angiogenesis. (A) Left panel: RT-PCR of MMP12 in control and VEGF-treated ECFCs. Right panel: Western blot analysis of MMP12 revealed in the culture medium of control and VEGF-treated ECFCs. (B) Matrigel invasion of control and VEGF-treated ECFCs, in the absence and in the presence of anti-MMP12 antibody (10 μg/mL), under basal conditions (control), and after VEGF stimulation. Histogram refers to quantification of Matrigel invasion assay obtained by counting the total number of migrated cells/filter. Results are the mean of 3 different experiments performed in triplicate in 3 ECFC preparations and are shown as mean value ± SD. *P < .05, significantly different from control. (C) Capillary morphogenesis of ECFCs using the same experimental conditions described for panel B. The figures are representative of a typical experiment of 3 experiments performed in triplicate in 3 ECFC preparations. Quantification was performed by measuring the percentage field occupancy of capillary projections, taking the control as 100%. *P < .05, significantly different from control. Image acquisition and quantification were performed as described in Figures 1 and 3.
Then, we demonstrated that MMP12 is involved in in vitro angiogenesis of ECFCs, both in basal conditions and after VEGF treatment (Figure 6B-C). Indeed, in the presence of MMP12 antibody in the culture medium (10 μg/mL), both migration and capillary morphogenesis were increased in control cells, whereas no differences were observed when MMP12 antibody was added to VEGF-treated cells, yet producing very low amounts of MMP12.
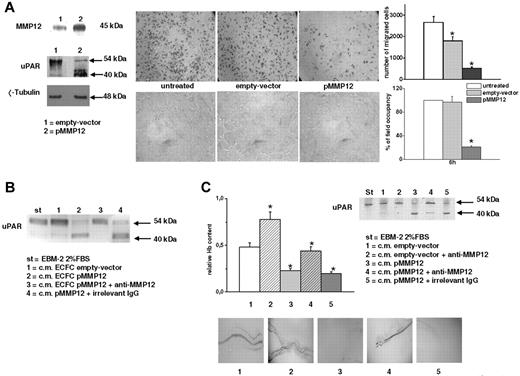
To demonstrate the consequence of uPAR cleavage on ECFCs angiogenesis, we transiently transfected ECFC with MMP12 and evaluated enzyme release in the medium and the presence of full-length and truncated uPAR in cell lysates. Figure 7A (left panels) shows that MMP12 overexpressing ECFCs efficiently truncated their own uPAR. MMP12 overexpression resulted in inhibition of ECFC Matrigel invasion and capillary morphogenesis (Figure 7A middle and right panels).
Effect of MMP12 transfection on in vitro and in vivo angiogenesis. ECFCs were transiently transfected with the recombinant vector pCDNA3.1 + MMP12. As control of transfection, empty vector pCDNA3.1 was used. (A) Left panel (top part): Western blotting analysis of MMP12 released in the medium from control and MMP12 transiently transfected ECFCs. Left panel (bottom part): truncation of uPAR in MMP12-transfected ECFCs. Numbers on the right show molecular weight expressed in kilodaltons. This figure shows typical results of 3 different experiments that gave similar results. The middle part of the figure shows Matrigel invasion (top panels) and capillary morphogenesis (bottom panels) of MMP12 transiently transfected ECFCs. Results are the mean of 3 different experiments performed in triplicate with 3 ECFC preparations. Histograms: Quantification of Matrigel invasion and capillary morphogenesis performed by counting migrated cells and percentage field occupancy of capillary projections, respectively. Image acquisition and quantification were performed as described in Figures 1 and 3. Results are shown as mean value ± SD. *P < .05, significantly different from control. (B) Western blotting showing MMP12-dependent uPAR cleavage. Standard uPAR (st) was incubated overnight with culture medium from control, empty vector and MMP12 transiently transfected ECFCs, in the absence or presence of anti-MMP12 antibody. st indicates standard uPAR incubated in EBM-2 medium with 2% FBS. Full-length and truncated forms of uPAR were evaluated by Western blotting analysis with the specific monoclonal antibody anti-uPAR M2. The figure shows the results of a typical experiment of 5 different experiments. (C) In vivo Matrigel sponge assay. Flanks of mice were injected with Matrigel (4 injections/animal) containing aliquots of 50 μL of reconstituted culture medium of ECFCs transfected with recombinant vector pCDNA3.1 + MMP12 or with pCDNA3.1 (empty vector), in the absence or in the presence of anti-MMP12 antibody (10 μg/mL), or of an irrelevant Ig. Top panels: Quantification of the experiment by evaluating hemoglobin (Hb) content of the sponges under the various experimental conditions (4 injections/animal; 2 animals for each condition). Graphs are shown as mean ± SD. *P < .05. Bottom panels: A representative photograph, taken with the Zeiss SR Stemi stereomicroscope, of the vascularization of individual Matrigel sponges recovered at autopsy for the corresponding condition and representative of a typical experiment. Image acquisition and quantification was performed as described in Figures 1 and 3. Inset (C top part): Western blotting of standard uPAR (st) incubated with aliquots of the solubilized plugs and then evaluated by Western blotting, using the M2 antibody (which recognizes both native and truncated uPAR forms). Only plug-extracted CM of pMMP12-ECFC cleaved uPAR. Such inhibition was counteracted by anti-MMP12 antibody but not by an irrelevant Ig, thus showing the specificity of anti-MMP12 antibodies. The figure shows a typical Western blotting pattern, of 5 experiments performed with different plugs extracts, that gave similar results.
Effect of MMP12 transfection on in vitro and in vivo angiogenesis. ECFCs were transiently transfected with the recombinant vector pCDNA3.1 + MMP12. As control of transfection, empty vector pCDNA3.1 was used. (A) Left panel (top part): Western blotting analysis of MMP12 released in the medium from control and MMP12 transiently transfected ECFCs. Left panel (bottom part): truncation of uPAR in MMP12-transfected ECFCs. Numbers on the right show molecular weight expressed in kilodaltons. This figure shows typical results of 3 different experiments that gave similar results. The middle part of the figure shows Matrigel invasion (top panels) and capillary morphogenesis (bottom panels) of MMP12 transiently transfected ECFCs. Results are the mean of 3 different experiments performed in triplicate with 3 ECFC preparations. Histograms: Quantification of Matrigel invasion and capillary morphogenesis performed by counting migrated cells and percentage field occupancy of capillary projections, respectively. Image acquisition and quantification were performed as described in Figures 1 and 3. Results are shown as mean value ± SD. *P < .05, significantly different from control. (B) Western blotting showing MMP12-dependent uPAR cleavage. Standard uPAR (st) was incubated overnight with culture medium from control, empty vector and MMP12 transiently transfected ECFCs, in the absence or presence of anti-MMP12 antibody. st indicates standard uPAR incubated in EBM-2 medium with 2% FBS. Full-length and truncated forms of uPAR were evaluated by Western blotting analysis with the specific monoclonal antibody anti-uPAR M2. The figure shows the results of a typical experiment of 5 different experiments. (C) In vivo Matrigel sponge assay. Flanks of mice were injected with Matrigel (4 injections/animal) containing aliquots of 50 μL of reconstituted culture medium of ECFCs transfected with recombinant vector pCDNA3.1 + MMP12 or with pCDNA3.1 (empty vector), in the absence or in the presence of anti-MMP12 antibody (10 μg/mL), or of an irrelevant Ig. Top panels: Quantification of the experiment by evaluating hemoglobin (Hb) content of the sponges under the various experimental conditions (4 injections/animal; 2 animals for each condition). Graphs are shown as mean ± SD. *P < .05. Bottom panels: A representative photograph, taken with the Zeiss SR Stemi stereomicroscope, of the vascularization of individual Matrigel sponges recovered at autopsy for the corresponding condition and representative of a typical experiment. Image acquisition and quantification was performed as described in Figures 1 and 3. Inset (C top part): Western blotting of standard uPAR (st) incubated with aliquots of the solubilized plugs and then evaluated by Western blotting, using the M2 antibody (which recognizes both native and truncated uPAR forms). Only plug-extracted CM of pMMP12-ECFC cleaved uPAR. Such inhibition was counteracted by anti-MMP12 antibody but not by an irrelevant Ig, thus showing the specificity of anti-MMP12 antibodies. The figure shows a typical Western blotting pattern, of 5 experiments performed with different plugs extracts, that gave similar results.
Because EPCs are recruited to sites requiring vascularization, such as ischemic tissues33 or tumors, where they contribute to the “angiogenic switch,”34 we evaluated whether ECFC MMP12 overproduction also influenced in vivo angiogenesis.
First, we evaluated uPAR cleavage by MMP12 released into the medium from transfected cells. We incubated standard uPAR with different CMs in the presence or absence of anti-MMP12 antibody and evaluated full-length and truncated uPAR by Western blotting with M2 antibody (Figure 7B). The control medium and the medium of empty vector-transfected ECFCs did not cleave uPAR, wheres CM of MMP12-transfected ECFCs produced truncated uPAR. Such truncation was inhibited by anti-MMP12 antibody, but not by irrelevant IgG.
We performed the Matrigel sponge assay in mice, using reconstituted ECFC CM from empty vector control (pCDNA3+ alone) or MMP12-transfected ECFCs, in the absence or presence of anti-MMP12 antibody. Vascularization was evaluated in recovered Matrigel sponges. We used the same medium that we experimentally demonstrated to contain high levels of active MMP12 and to be able to truncate uPAR (Figure 7B). Groups of 4 pellets were injected for each treatment. Individual Matrigel sponges were recovered at autopsy 5 days after implants. As shown in Figure 7C, whereas angiogenesis was stimulated by medium from empty vector control, it was inhibited by MMP12-expressing ECFCs, as shown also by decrease in sponge hemoglobin content. This inhibitory effect was the result of the enzymatic activity of released MMP12 as it was reverted by anti-MMP12 antibody but not by an irrelevant IgG.
To still further confirm these results, we tested the MMP12 activity within the recovered Matrigel sponges. We demonstrated that the standard uPAR cleaving activity persisted in the sponges containing CM of MMP12-transfected ECFCs (Figure 7C inset). Such activity was inhibited by anti-MMP12 antibody but not by irrelevant IgG, thus demonstrating the specificity of this effect.
Discussion
In this study, we demonstrated that the angiogenic properties of ECFCs depend on the integrity of caveolae and on the presence of full-length uPAR in such specialized membrane structures. We also showed that uPAR is an inducer of caveolar raft organization and that uPAR integrity in caveolae is promoted by VEGF by a decrease of MMP12-dependent uPAR truncation. Further, MMP12 overexpression inhibited vascularization in vitro and in vivo.
uPAR is anchored to the cell membrane through a glycosylphosphatidylinositol tail, which accounts for its presence in “lipid rafts.” Caveolae are specialized lipid rafts, particularly abundant in ECs. Our aim to investigate a possible correlation between caveolar rafts, distribution of full-length and truncated forms of uPAR, and angiogenesis in ECFCs relies on its identification in caveolae13 and on the recognized role of full-length uPAR in angiogenesis.10,11,31,32,35 Here, we used UCB ECFCs because of their biologic properties5 : ECFCs display a higher proliferative rate compared with mature ECs, form secondary and tertiary colonies on replating and de novo blood vessel formation in vivo,36 and can be obtained by a noninvasive method and then expanded ex vivo to achieve a considerable number of cells.
We observed that in unstimulated ECFCs uPAR distributes mainly in nonraft fractions of the membrane. VEGF stimulation up-regulated both caveolin-1 and uPAR inducing, at the same time, a shift of full-length uPAR from the nonraft fraction to caveolae. Integrity of caveolae is essential in many cellular functions,29,30 including angiogenesis. We observed that ECFC caveolae disruption by β-MCD or caveolin-1 silencing induced cell membrane uPAR redistribution outside of caveolae and that uPAR silencing impaired a normal caveolae organization, thus indicating a role of uPAR as a caveolar raft organizer.
Studies on caveolin-1 emphasize a paradoxical function of caveolin in angiogenesis promotion/inhibition18 in given cellular and animal models, which are restriction of EC hyperproliferation in undifferentiated EC and promotion of migration/differentiation of EC in mature vessels. In line with a positive role of caveolin-1 in the migration/differentiation steps of angiogenesis, our data show that VEGF stimulation of ECFCs induces a caveolin-dependent ERK1/2 phosphorylation, which is considered the terminal signaling event in EC migration/differentiation after VEGF challenge. Moreover, our data further support the principle that integrity of caveolae structure is critical for accurate VEGF-induced signaling.37
Further, immunofluorescence has indicated that the number and size of caveolar clusters and uPAR/caveolin-1 colocalization increased under the effect of VEGF, whereas the same parameters decreased on chemical disruption of caveolae.
We observed that the treatment of ECFCs with β-MCD, as well as caveolin silencing, impaired Matrigel invasion and capillary morphogenesis, thus demonstrating that integrity of caveolae affects the angiogenic properties of ECFCs in vitro. To evaluate the role of caveolar raft uPAR, we performed angiogenic assays by uPAR gain/loss of function. Stimulation of ECFCs with VEGF, which we demonstrated to up-regulate caveolin-1 and uPAR and to promote partition of full-length uPAR in caveolae, caused an increase of Matrigel invasion and capillary morphogenesis, inhibited by anti-uPAR antibodies. In addition, silencing of uPAR gene using anti-uPAR aODNs, which inhibit uPAR expression and caveolae formation, resulted in impairment of ECFC Matrigel invasion and capillary morphogenesis. These results demonstrated that integrity of caveolae influences the angiogenic properties of ECFCs and that caveolar uPAR is critical in ECFC-dependent angiogenesis.
Overall, these results demonstrate that uPAR-mediated caveolae formation is required for ECFC angiogenesis, which is inhibited by uPAR silencing, by β-MCD treatment which disrupt caveolae and induces uPAR redistribution outside of caveolae, and by caveolin-1 silencing.
uPAR has been shown to play a major role in VEGF-induced EC migration/invasion, as VEGF leads to uPA–PAI-1–uPAR complex formation, which is internalized via low-density lipoprotein receptor-like proteins and is thereafter redistributed to the leading edge of migrating cells. Our results open the question of whether uPAR redistribution to caveolae is performed via lateral shift or via an low-density lipoprotein receptor-dependent internalization and recycling process. The latter one is suggested by the observation that truncated uPAR is not found in lipid rafts and that uPAR needs to be in its full-length to recycle through this pathway.38
On the basis of our previous studies10,11 showing that the MMP12-dependent uPAR cleavage severely impaired angiogenesis, we evaluated a possible role of MMP12 in ECFC angiogenesis. We demonstrated that the increased angiogenic ability of VEGF-treated ECFCs is related both to uPAR up-regulation and to its lower cleavage because of the decreased levels of MMP12 and that MMP12 overproduced by transfected ECFCs cleaves uPAR and reduces ECFC angiogenic performance in vitro.
In vivo experiments demonstrated that culture medium of MMP12-transfected ECFCs inhibited vascularization of the Matrigel sponge in mice, which was counteracted by anti-MMP12 antibody, suggesting that ECFC-induced angiogenesis in vivo depends on the presence of the full-length uPAR.
Although many studies evaluating the therapeutic potential of EPCs in neovascularization in cardiovascular disease39 and in systemic sclerosis40,41 have reported conflicting results, these cells represent a hope for therapy. Loss of function of MMP12 in injected EPCs, alone or together with induction of uPAR up-regulation by VEGF stimulation, could be evaluated as good strategy for vascular therapy.
The possibility to reduce angiogenesis through the “loss of function” of uPAR could be important to control excessive angiogenesis, such as in tumors. Indeed, many studies suggest an important role of EPCs in tumor vascularization and metastasis by incorporation in vessels and/or by supporting angiogenesis via paracrine secretion of proangiogenic cytokines.34,42 Limited work has been performed on the ability of human ECFCs to regenerate the vascular system in preclinical studies,43 and on their role in tumor angiogenesis. However, our Matrigel sponge data indicate that, if ECFCs are able to reach a site of vascularization, they can significantly influence EC angiogenesis. Therefore, ECFCs could be used as cellular vehicles to deliver anticancer agents.44 A possibility for cancer therapy could be to manipulate ECFCs to deliver MMP12 into the tumor mass with the aim to truncate uPAR both in ECs and tumor cells, thus inhibiting tumor angiogenesis, growth, and metastasis, features that require an intact native uPAR. Our data showing that caveolae concentrate a functional form of uPAR, that is critical for the invasion process, provide a possible explanation to new attempts to control cancer cell spreading based on administration of statins that modify lipid rafts by reducing membrane cholesterol.45 Because statins are safe and orally available agents, they may enlarge the range of their indications also through their angiogenic modulating effect.46,47
Our data suggest that a combined therapy based on cholesterol-depleting agents and uPAR loss of function could be a promising approach in the control of tumor spreading and growth.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by Ministero Italiano dell'Università e della Ricerca Scientifica, Ente Cassa di Risparmio di Firenze, Toscana Life Sciences, and Istituto Toscano Tumori.
This work is in memory of Professor Mario Serio.
Authorship
Contribution: F.M., A.C., and S.S. performed in vitro experiments; A.L., L.C., and F.B. performed in vivo experiments; B.M., R.S., and M.S. prepared ECFCs; L.M. and L.P. performed immunofluorescence experiments; G.D., N.S., and F.R. performed immunofluorescence analysis; and M.D.R. and G.F. designed the research and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Gabriella Fibbi, Department of Experimental, Pathology and Oncology, Viale G.B. Morgagni 50, 50134 Florence, Italy; e-mail: fibbi@unifi.it; and Mario Del Rosso, Department of Experimental, Pathology and Oncology, Viale G.B. Morgagni 50, 50134 Florence, Italy; e-mail: delrosso@unifi.it.
References
Author notes
F.M. and A.C. contributed equally to this study.