Abstract
Abstract 1033
Paroxysmal nocturnal hemoglobinuria (PNH) is a chronic and life-threatening hematopoietic stem cell disorder characterized by deficiency of the GPI-anchored complement inhibitory proteins CD55/59. Chronic hemolysis from this deficiency leads to serious clinical morbidities including thromboembolism, chronic kidney disease, and increased mortality. The International Clinical Cytometry Society (ICCS) recommends multiparameter high sensitivity flow cytometry (HSFC) as the method of choice for diagnosing PNH. The ICCS also provides guidance on the clinical indications for testing for PNH, including patients (pts) with bone marrow failure (BMF), unexplained cytopenias, unexplained thrombosis, hemoglobinuria and hemolysis.
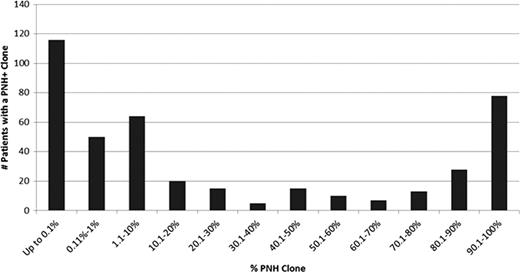
The aim of this study is to use HSFC with sensitivity up to 0.01% to analyze 6,897 pts who were screened for PNH clones utilizing CD235a/CD59 for RBCs, FLAER/CD24/CD15/CD45 for neutrophils and FLAER/CD14/CD64/CD45 for monocytes. We evaluated the clinical indications for PNH testing with the provided ICD-9 diagnostic (DX) codes and examined the change in PNH clone sizes among pts who had follow-up studies in 3–12 months.
Incidence of PNH Clones in Patients with ICD-9 Diagnostic Code at Dahl-Chase Diagnostic Services
| ICD-9 Diagnostic Code . | General Description . | Incidence of PNH Clone . |
|---|---|---|
| 284, 284.01, 284.8, 284.81, 284.89, 284.9 | Aplastic Anemia | 26.3% (94/357) |
| 238.7, 238.72, 238.73, 238.74, 238.75, 238.76 | Myelodysplastic Syndrome (MDS) | 5.5% (32/585) |
| 287.5 | Unexplained Cytopenia | 5.7% (13/230) |
| 284.1 | Pancytopenia | 6.0% (63/1058) |
| 285.2, 285.21, 285.29, 285.9 | Anemia Unspecified | 3.6% (40/1122) |
| 283, 283.1, 283.10, 283.11, 283.19, 283.2, 283.9 | Hemolytic Anemia | 22.7% (147/647) |
| 791, 791.2 | Hemoglobinuria | 18.9% (14/74) |
| 790.6, 790.99, 790.4 | Hemolysis | 7.9% (18/227) |
| 325, 415.1, 415.11, 434, 434.01, 444.22, 451.11, 451.19, 452, 453, 453.0, 453.2, 453.4, 453.41, 453.89, 453.9, 557, 557.1 | Thrombosis | 1.4% (14/967) |
| 280.9 | Unspecified Iron Deficiency | 2.5% (7/278) |
| Other ICD-9 diagnostic codes | 2.1% (26/1232) | |
| Not Provided | 4.8% (51/1065) |
| ICD-9 Diagnostic Code . | General Description . | Incidence of PNH Clone . |
|---|---|---|
| 284, 284.01, 284.8, 284.81, 284.89, 284.9 | Aplastic Anemia | 26.3% (94/357) |
| 238.7, 238.72, 238.73, 238.74, 238.75, 238.76 | Myelodysplastic Syndrome (MDS) | 5.5% (32/585) |
| 287.5 | Unexplained Cytopenia | 5.7% (13/230) |
| 284.1 | Pancytopenia | 6.0% (63/1058) |
| 285.2, 285.21, 285.29, 285.9 | Anemia Unspecified | 3.6% (40/1122) |
| 283, 283.1, 283.10, 283.11, 283.19, 283.2, 283.9 | Hemolytic Anemia | 22.7% (147/647) |
| 791, 791.2 | Hemoglobinuria | 18.9% (14/74) |
| 790.6, 790.99, 790.4 | Hemolysis | 7.9% (18/227) |
| 325, 415.1, 415.11, 434, 434.01, 444.22, 451.11, 451.19, 452, 453, 453.0, 453.2, 453.4, 453.41, 453.89, 453.9, 557, 557.1 | Thrombosis | 1.4% (14/967) |
| 280.9 | Unspecified Iron Deficiency | 2.5% (7/278) |
| Other ICD-9 diagnostic codes | 2.1% (26/1232) | |
| Not Provided | 4.8% (51/1065) |
Note: Table reflects patients who had more than one ICD9 code associated with their laboratory tests.
In this single-laboratory experience, we evaluated the incidence of PNH in these high risk groups. In this study, 26.3% of pts with the diagnosis of BMF had PNH+ clones detected, underscoring the need to test this group of pts. The study confirmed the utility of testing pts with unexplained hemolytic anemia, hemolysis and hemoglobinuria where the combined rate of positivity was 48%. In addition, this study highlights the need to monitor pts with small PNH clones by HSFC analysis as these pts may show significant variation over time. This examination of ICD-9 DX code association with presence of PNH+ clones confirms the need to actively test high risk populations for PNH based on the ICCS recommendations to ensure accurate diagnosis and early intervention.
Weitz:Alexion Pharmaceuticals, Inc.: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Illingworth:Dahl-Chase: Employment; Alexion: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.