Abstract
Abstract 1578
It is known that advanced disease in diffuse large B-cell lymphoma (DLBCL) confers a poor prognosis, and staging investigations are routinely performed at diagnosis, including a bone marrow biopsy. Several studies have suggested that histologically proven bone marrow involvement with DLBCL is an independent predictor of a poor prognosis. However, the clinical role of flow cytometry in staging bone marrow in DLBCL, especially its impact on outcome, remains uncertain. The aim of this study is to evaluate the incidence of occult bone marrow involvement which is detectable only by flow cytometry, and examine the significance of occult bone marrow involvement in patients treated with R-CHOP.
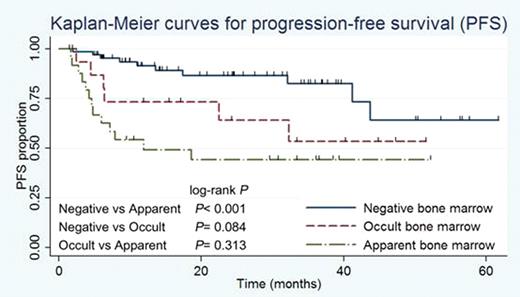
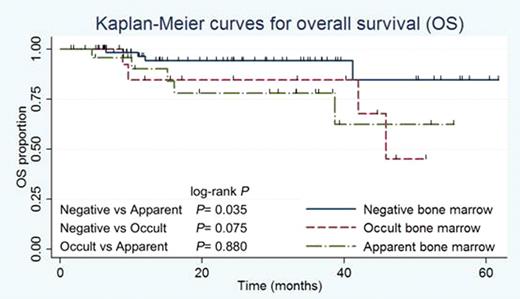
This is a retrospective pooled analysis of unselected patients with DLBCL treated with R-CHOP in our institute. Patients were included in the analysis if they were with a biopsy proven diagnosis of DLBCL and had undergone a pretreatment bone marrow aspiration, which was examined both by immunohistochemistry and by flow cytometry. By using flowcytometry, DLBCL involvement was defined by the significant bias in the ratio of kappa and lambda harboring large cells in CD19-gated lymphocytes, indicating occult bone marrow involvement of DLBCL. All patients were divided into three groups; those with histologically apparent bone marrow involvement, those with occult bone marrow involvement and those with a negative bone marrow. This was an intention-to-treat analysis, including all patients treated with curative intent who received at least one cycle of R-CHOP. Clinical characteristics between each group were analyzed. Progression-free survival (PFS) and overall survival (OS) were assessed using the Kaplan-Meier method and the log-rank test was used for comparison between each group. A multivariate Cox regression analysis was used to adjust for IPI score.
From April 2005 to February 2011, 105 consecutive patients with DLBCL received staging bone marrow aspiration. Among them, 25 (23.8%) had histologically apparent lymphoma involvements and 65 (61.9%) showed undetectable lymphoma cells. In remaining 15 patients (14.3%), examination of smear preparation and clot section could not find lymphoma cells, however, flow cytometry revealed significant bias in the ratio of kappa and lambda harboring cells in CD19-gated lymphocytes. At the time of analysis, median follow-up time for living patients was 26 months (range, 2–61). PFS and OS in those with histologically apparent bone marrow involvement were significantly inferior than in those with negative bone marrow involvement (3-year PFS 44.3% for apparent group vs 82.5% for negative group, log-rank P < 0.001; 3-year OS 78.2% for apparent vs 94.1% for negative, log-rank P = 0.035). Difference in 3-year PFS and OS between occult (53.5% and 84.6%, respectively) and negative bone marrow involvement groups were not significant, but there was a tendency for occult bone marrow involvement group to have a shorter PFS and OS when compared to negative bone marrow group (log-rank P = 0.084 and 0.075, respectively). Moreover, when occult cases were included with apparent cases as a positive bone marrow group, difference in OS between positive and negative bone marrow groups was significant (3-year OS 80.9% for positive vs 94.1% for negative group, log-rank P = 0.022), whereas when occult cases were included with negative cases as negative bone marrow group using the conventional definition by morphology alone, difference in OS between histologically positive and negative bone marrow groups was not significant (3-year OS 78.2% for positive vs 92.3% for negative group, log-rank P = 0.095). In a multivariate analysis, apparent but not occult bone marrow involvement remained a significant prognostic value in PFS independent of IPI score (relative risk 3.0, 95% CI 1.1–8.5, P = 0.0296).
Taking all into account, occult bone marrow involvement has potentially adverse impact on the outcome in DLBCL treated with R-CHOP. The threshold of the ratio of lymphoma cells among bone marrow nucleated cells which have great impact on clinical outcome should be defined.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.