Abstract
Abstract 1581
LR11 is a type I membrane protein from which a large extracellular part, soluble LR11 (sLR11), is released by proteolytic shedding. It plays a key role in the migration of undifferentiated vascular smooth muscle cells, and circulating sLR11 is a known biomarker of carotid intima-media thickness. We have recently found that LR11 is specifically and highly expressed on the cell surface of acute leukemia cells in addition to normal leukocytes. Furthermore, patients with various hematological malignancies showed significantly high serum sLR11 levels especially in B-cell acute lymphoblastic leukemia. Serum sLR11 level has a significant association with remission and survival rate in patients with acute leukemia (Ohwada et al. 2010 ASH annual meeting). Based on these findings, we have retrospectively evaluated the clinical importance of serum sLR11 in patients with diffuse large B cell lymphoma (DLBCL) and follicular lymphoma (FL).
Fifty-one patients with DLBCL and 23 patients with FL treated at Chiba University Hospital between 2002 and 2011 were evaluated. The majority of patients were treated by the R-CHOP regimen (rituximab 375 mg/m2 on day 1; cyclophosphamide, 750 mg/m2 on day 1; adriamycin, 50 mg/m2 on day 1; vincristine, 1.4 mg/m2 on day 1; and prednisolone, 100 mg/body on day 1–5). Patient biopsy specimens were subjected to immunostaining using anti-LR11 antibody. Serum sLR11 levels were measured by ELISA. Patient laboratory data and treatment outcome were obtained retrospectively.
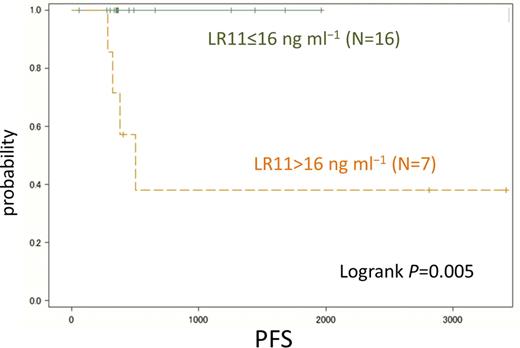
Immunostaining of paraffin-embedded lymphoma tissue revealed that the cytoplasm of lymphoma cells of both DLBCL and FL specifically reacted against the anti-LR11 antibody. Furthermore, serum sLR11 levels of patients with lymphoma were significantly increased (DLBCL: 17.4±14.7 ng ml−1, FL: 22.7±25.5 ng ml−1) compared with those of normal control subjects (8.8±1.79 ng ml−1, P <0.0001). Paired sample analysis of patients at complete remission after chemotherapy showed significantly decreased sLR11 levels compared with that at the time of diagnosis (DLBCL: 13.6 ± 8.4 ng ml−1 vs. 10.8 ± 5.9 ng ml−1, P =0.045; FL: 20.0 ± 26.4 ng ml−1 vs. 7.4 ± 1.8 ng ml−1, P =0.0019). Multiple stepwise linear regression analysis showed that the serum sLR11 level at diagnosis was independently associated with bone marrow invasion in patients with DLBCL and bone marrow invasion and elevated LDH levels in patients with FL (DLBCL: r2 = 0.33, P =0.037, FL: r2 = 0.51, bone marrow invasion: P =0.0067, elevated LDH levels: P =0.013). Four of 7 patients with FL and high (≥16 ng ml−1) sLR11 levels relapsed, while none of the 16 patients with FL and low (≤16 ng ml−1) sLR11 did. The relapse rate was significantly higher in patients with FL and serum sLR11 levels ≥16 ng ml−1 (0% vs. 57%, P<0.004). At the median follow-up period of 13.5 months, the probability of 5-year progression-free survival (PFS) was significantly higher in patients with sLR11 >16 ng ml−1 at diagnosis compared with those with ≤16 ng ml−1 (Figure 1, 38.1 % vs 100 %, P =0.005). Stepwise Cox regression analysis showed that high serum sLR11 at diagnosis was the only independent risk factor associated with PFS in patients with FL.
sLR11 was demonstrated to be expressed in B cell lymphoma cells by immunohistochemistry. Elevated serum sLR11 levels were associated with bone marrow invasion, and they significantly decreased to normal range after the remission. These findings suggest that sLR11 is a novel biomarker derived from lymphoma cells, which reflects not only tumor burden but also its migration and attachment activities, translating into inferior PFS in patients with FL. Although the number of patients in this study was limited, serum sLR11 can be a promising biomarker in patients with B cell lymphoma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.