Abstract
Abstract 1630
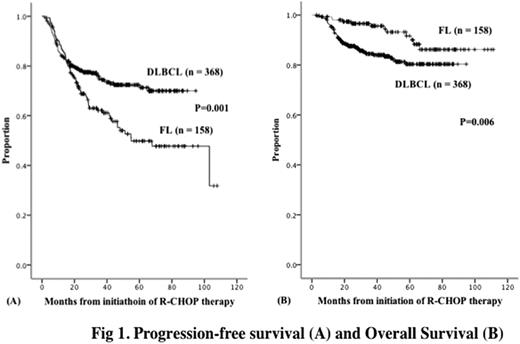
In almost all cases, follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL) are CD20 positive. Since the introduction of rituximab (R), the outcome of the patients with FL or DLBCL has improved perceptively. Since 2001 and 2003, the Yokohama City University Hematology Group in Japan has uniformly treated FL and DLBCL patients, respectively, with 6 cycles of standard (21 days) R-CHOP therapy with curative intent, except in the case of stage 1 FL. Here, we report our experience. Patients and Methods: Five hundred and twenty-six untreated consecutive patients (158, FL; 368, DLBCL) between 2001 and 2009 were the subjects of this study. All the patients were scheduled to undergo primary therapy with 6 cycles of full-dose R-CHOP in our 7 hospitals. Patients who had partial remission (PR) after the 4 initial cycles were administered a total of 8 R-CHOP cycles. Patients who did not achieve PR after the 4 initial R-CHOP cycles or those with disease progression at any given time received salvage therapy, and that time point was designated as the point at which the disease had started progressing. Patients who required more than 20% dose reduction were excluded from the study. Those with special forms of DLBCL, such as intravascular lymphoma, primary mediastinal large B-cell lymphoma, and T-cell-rich B-cell lymphoma, were also excluded. Additional local irradiation was performed in patients with PR or complete remission (CR) if deemed necessary by the attending physician. No patients received maintenance therapy with R. DLBCL patients who achieved CR but were initially at risk of central nervous system (CNS) involvement received methotrexate (15 mg) and hydrocortisone (25 mg) 4 times intrrathecally for CNS prophylaxis. Central pathological reviews were not performed; only the individual institutional diagnoses were used. Results: In the cases of FL, the pathological grading was grade 1 for 65 patients, grade 2 for 61 patients, grade 3a for 20 patients, and grade 3b for 12 patients. There were 81 men and 77 women, and the median age at diagnosis was 57 years (range, 25–76). In accordance with the International Prognostic Index (IPI), 60 patients were at low risk (L); 60, at low-intermediate risk (LI); 26, at high-intermediate risk (HI); and 12, at high risk (H). According to the Follicular Lymphoma IPI, 43 patients were classified as L; 49, as being at intermediate risk; and 59, as H. For 7 patients, the risk was undetermined. Ten patients received additional local irradiation in PR/CR at the end of the R-CHOP therapy. None received CNS prophylaxis. Twelve deaths were observed among the FL patients, 10 of which were due to the lymphoma. In the DLBCL group, there were 209 men and 159 women, and the median age at diagnosis was 64 years (range, 18–80). According to the IPI, 158 patients were classified as L; 93, as LI; 57, as HI; and 60, as H. Thirty-seven patients received additional local irradiation in PR/CR at the end of the R-CHOP therapy. CNS prophylaxis was performed in 42 patients who had an initial CNS risk and achieved CR. In the observaton period, there were 58 deaths among the DLBCL patients, 50 of which were due to the lymphoma. The median observation period for the living patients with FL and DLBCL was 45 months and 43 months, respectively. For the FL group, the CR, 5-year progression-free survival (PFS), and 5-year overall survival (OS) rates were 86%, 50%, and 92%, respectively. Between patients with grade 1–2 FL, and grade 3 FL, the PFS (P = 0.16) and OS (P = 0.17) were not significantly different. This was found to also be true when the PFS (P = 0.19) and OS (P = 0.32) of grade 1–3a and grade 3b FL patients were compared. For the DLBCL group, the CR, 5year PFS, and 5-year OS rates were 89%, 72%, and 80%, respectively. The PFS rate was significantly higher in the DLBCL group compared to the FL group (Fig 1(A), P = 0.001), but the OS was significantly greater in the FL group (Fig 1(B), P = 0.006). Conclusion: Standard R-CHOP therapy is effective for patients with FL and DLBCL, with the 5-year OS rate exceeding 80% for both. However, in the FL group, the PFS did not show a plateau, suggesting the incurability of this lymphoma with R-CHOP therapy. The good OS indicated the effectiveness of salvage therapy for FL patients. Since the OS and PFS in patients with grade 3 FL were similar to those in patients with grade 1–2 FL, all grades of FL should probably be categorized simply as “FL” with regard to R-CHOP therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.