Abstract
Abstract 1707
Treatment of pts with higher-risk MDS revolves around AHSCT and HMA. Although AHSCT is thought to be the only curative approach for pts with MDS, only a small percentage of pts are appropriate candidates and this procedure carries significant morbidity and mortality rates. We wanted to assess outcomes in pts with higher risk MDS treated with AHSCT or HMA. To study this, we performed a retrospective analysis comparing the outcome of pts with previously untreated MDS who received AHSCT or HMA therapy at M.D. Anderson Cancer Center (MDACC).
From a database of pts with MDS who received AHSCT (N=152) at MDACC between 01/1988 and 04/2008, we selected those with untreated MDS prior to receiving the transplant. A total of 53 (29%) pts were identified. We compared them with a control group of 40 pts treated with HMA among 1748 referred to MDACC. All controls were selected to match at least 3 of the following 5 criteria: 1) age, 2) year of diagnosis, 3) percentage of blasts at the time of diagnosis, 4) IPSS cytogenetic risk, and 5) time from diagnosis to treatment. The primary endpoint was survival.
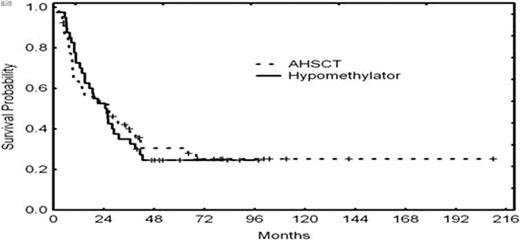
A total of 53 pts with untreated MDS who received AHSCT and 40 pts treated with HMA were identified (Table 1). Median age was 51 (range 20–62) and 54 (range 38–79) years for pts treated with AHSCT or HMA respectively. There were more pts greater than 60 years old in the HMA group compared to those in the AHSCT group (58% vs. 1% p>0.001). The median follow up time was 64 months. Donors were HLA matched related (n=37), matched unrelated (n=11), 1 antigen mismatched related (n=4) or 1 antigen mismatched unrelated (n=1). Of the 40 pts treated with HMA, 31 were evaluable for response; of those 31, 19 (61%) responded, 16 (52%) achieving a complete response. The median survival was 26 and 25 months for pts receiving AHSCT or HMA, respectively (p=0.41) (Figure 1). The 8-year overall survival rates for pts receiving AHSCT or HMA were 24% and 23% respectively.
| . | AHSCT . | HMA . | p-value . |
|---|---|---|---|
| Age (years) | 51 | 54 | <0.001 |
| Median | 20-62 | 38-79 | |
| Range | 3 | 23 | |
| Age >60 | |||
| Sex | 31 | 23 | NS |
| Male | 22 | 17 | |
| Female | |||
| IPSS CG | 15 | 10 | NS |
| Good | 5 | 4 | |
| Intermediate | 33 | 26 | |
| Poor | |||
| IPSS BM Blasts | 32 | 22 | NS |
| <5% | 17 | 15 | |
| 5-10% | 4 | 3 | |
| 11-20% | |||
| Hemoglobin (g/dL) | 29 | 22 | NS |
| <10 | 24 | 18 | |
| >10 | |||
| Platelets (x 109/L) | 36 | 29 | NS |
| >100 | 17 | 11 | |
| <100 | |||
| WBC (x 109/L) | 49 | 34 | NS |
| >5 | 4 | 6 | |
| <5 | |||
| Prior malignancies | 28 | 21 | NS |
| Yes | 25 | 19 | |
| No | |||
| TOTAL | 53 | 40 |
| . | AHSCT . | HMA . | p-value . |
|---|---|---|---|
| Age (years) | 51 | 54 | <0.001 |
| Median | 20-62 | 38-79 | |
| Range | 3 | 23 | |
| Age >60 | |||
| Sex | 31 | 23 | NS |
| Male | 22 | 17 | |
| Female | |||
| IPSS CG | 15 | 10 | NS |
| Good | 5 | 4 | |
| Intermediate | 33 | 26 | |
| Poor | |||
| IPSS BM Blasts | 32 | 22 | NS |
| <5% | 17 | 15 | |
| 5-10% | 4 | 3 | |
| 11-20% | |||
| Hemoglobin (g/dL) | 29 | 22 | NS |
| <10 | 24 | 18 | |
| >10 | |||
| Platelets (x 109/L) | 36 | 29 | NS |
| >100 | 17 | 11 | |
| <100 | |||
| WBC (x 109/L) | 49 | 34 | NS |
| >5 | 4 | 6 | |
| <5 | |||
| Prior malignancies | 28 | 21 | NS |
| Yes | 25 | 19 | |
| No | |||
| TOTAL | 53 | 40 |
AHSCT did not offer a significant survival improvement in a retrospective analysis of pts with MDS. Treatment with a HMA offers an adequate alternative in older patients or those who cannot tolerate or receive an AHSCT and should be used as a bridge in younger pts who are candidates for AHSCT
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.