Abstract
Reduced intensity conditioning (RIC) regimens in umbilical cord blood transplant (UCBT) are increasingly utilized for older patients (pts) and those with comorbidities. However, the optimal conditioning regimen has not yet been established and remains a significant challenge of this therapeutic approach. Incorporation of ATG into the conditioning regimen is thought to decrease the incidence of graft rejection, but it is associated with high incidence of infusion associated reactions and serum sickness, delayed T cell recovery, increased infections and higher risk of EBV post-transplant lymphoproliferative disorder (PTLD). We report the results of a non-ATG containing RIC regimen, in which ATG is replaced with a higher dose of TBI in pts considered to be at higher risk of graft failure.
All pts received fludarabine (40mg/m2/day) from day −6 to day −2 and cyclophosphamide (50mg/kg) on day −6. Pts who had received a previous autologous transplant within 12 months or ≥ 2 cycles of multiagent chemotherapy with at least one cycle of therapy within the 3 months previous to UCBT received a single fraction of 200cGy TBI on day −1. All other pts were considered at higher risk of graft rejection and received a single fraction of 300cGy of TBI on day −1. GVHD prophylaxis began on day −3 and consisted of cyclosporine A (CSA) and mycophenolate mofetyl (MMF). CSA was continued until at least day +100 and then tapered 10% per week starting on day +101 and discontinued no sooner than 6 months post-transplant. The duration of MMF was prolonged, with initiation of a taper on day+40 post transplant and then in the absence of GVHD, tapered by 12% per week and discontinued after day + 96.
Thirty pts underwent double UCBT at 3 transplant centers using this protocol between February 2006 and January 2011. Median age and weight of the pts were 60 (range, 24–73) years and 78 (range, 55–141) kg, respectively. Disease status included AML-CR1 (n=11) and CR2 (n=5), ALL-CR2 (n=1) and refractory ALL (n=2), biphenotypic leukemia in 1st CR (n=1), MDS (n=1), relapsed/ refractory Hodgkin lymphoma (n=3), transformed DLBCL (n=1), primary PTCL (n=1) and very high grade B cell lymphoblastic lymphoma in 2nd CR (n=1). Nine pts (30%) had failed prior hematopoietic cell transplantation (HCT), of which 5 were auto, 3 were allo and 1 both auto and allo transplant. All pts received 2 cord blood units to achieve the required cryopreserved cell dose of 3.0×107 TNC/kg. The median cell doses infused were 4.92 × 107 (range, 3.12–8.3) TNC/kg and 0.26×106 (range, 0.02–2.85) CD34+ cells/kg. Among the 60 infused units, HLA matching was 6/6 in 3% (n=1), 5/6 in 30% (n=9) and 4/6 in 67% (n=20) of the pts. Twenty-two pts (73%) received 2GY and 8 (27%) received 3Gy of TBI. The median number of prior treatments and comorbidity score were 3 (range, 0–8) and 3 (range, 1–8), respectively. The median follow up was 183 days (range, 132 to 1303 days).
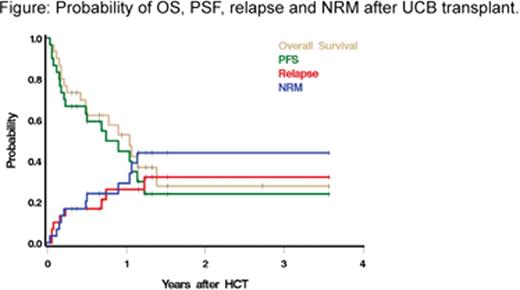
Neutrophils engraftment occurred in all pts at a median of 13 (range, 6 to 40) days and platelet (PLT) engraftment (>50×109/L ) occurred at a median of 32 (range, 23 to 42) days, respectively. There was only one case of secondary graft rejection and no cases of primary graft rejection. The cumulative incidence of acute GVHD grade II-IV and III-IV were 60% and 24%, respectively; the cumulative incidence of chronic GVHD was 18%. Day 100 NRM was 17%. At one year, NRM, OS and PFS were 29%, 53% and 45%, respectively. Causes of death included relapse (n=6), multi-organ failure (n=2), sepsis (n=1), diffuse alveolar hemorrhage (n=1), necrotizing hemorrhagic meningitis (n=1), leukoencephalopathy (n=1) and intracranial bleed (n=1).
There were no cases of CMV disease or PTLD. On multivariate analysis, only neutrophil and platelet engraftment were associated with mortality, with hazard ratios of 0.07 (95%, CI 0.009–0.61), p=0.01) and 0.11 (95%, CI 0.03–0.41, p=0.0009), respectively. Other variables, such as age, number of previous regimens, presence of minimal residual disease prior to transplant, dose of TBI (3Gy vs 2Gy), high-risk disease, comorbidity score and acute GVHD grade II-IV were not statistically significantly associated with poorer survival.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.