Abstract
Transplant options are limited for adult patients (pts) who lack a fully matched related or unrelated donor. We hypothesized that in-vivo T-cell depletion with r-ATG would allow safe allo-SCT from mismatched, unrelated donors, thus expanding the potential donor pool for pts with hematologic malignancies who require allo-SCT.
Thirty seven adult pts (age 20 – 70, median 45) underwent a first unrelated, mismatched, allo-SCT between 1/1/2006 and 6/30/2011 at Mayo Clinic Arizona for hematologic malignancy (35 PBSC, 2 marrow). All pts had at least a one allele or one antigen mismatch (MM) at HLA-A, -B, -C, or -DRB1, and all except one pt received r-ATG as part of the GVHD prophylaxis strategy (dose range 2.5 – 10 mg/kg in daily dose of 2.5 mg/kg depending on degree of mismatch, with the last dose generally given on day −1). One pt received Campath after experiencing anaphylaxis to r-ATG. Pts were transplanted for acute myeloid leukemia (n = 19; 10 CR1, 6 CR2, 3 other), acute lymphoblastic leukemia (n = 8; 4 CR1, 4 CR>/= 2), chronic myeloid leukemia (n = 1), myelodysplastic syndrome (n = 5), or non-Hodgkin lymphoma (n = 4). Conditioning was myeloablative in 20, reduced intensity in 16, and non-myeloablative in 1. Mismatches were as follows: 1-allele MM (n = 7); 1 antigen MM (n = 15); 2 allele MM (n = 4); 1 antigen, 1 allele MM (n = 7); and 2 antigen MM (n = 4). Additional GVHD prophylaxis included tacrolimus plus either methotrexate (n =21), mycophenolate mofetil (n = 14), or other (n = 2).
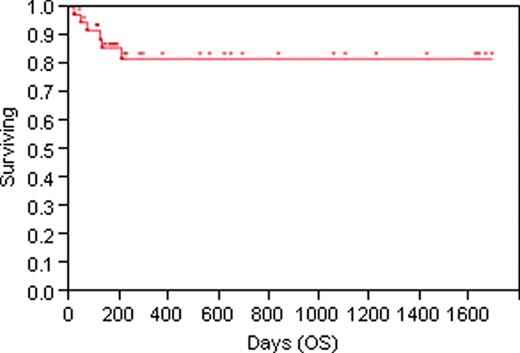
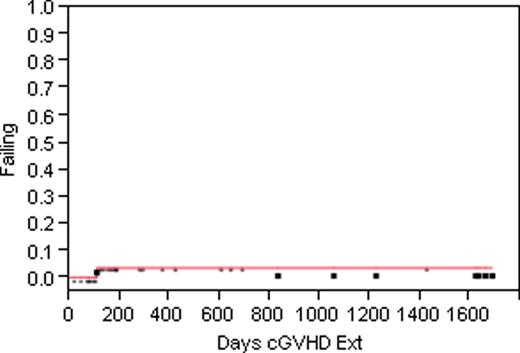
The median follow-up for surviving pts is 12 months. As of 6/30/11, 31 pts were alive, and 6 had died of the following causes: multiorgan failure (n = 1), relapse (n = 3), and veno-occlusive disease (n = 2). To date, there have been no deaths related to acute or chronic GVHD. The 1- and 2-year estimated rates of overall survival are 84.5%/78.8% (Fig. 1); of progression-free survival 79.7%/72.0%. The estimated rate of relapse at 1 and 2 years is 11.8%/18.7%, and of non-relapse mortality 8.1%/10.5%. Four pts (10.8%) have developed severe (grades III-IV) acute GVHD by day 100 (days 19, 27, 30, 43; one pt after withdrawal of prograf due to transplant-associated microangiopathy). No late onset severe acute GVHD has been seen. Moderate to severe NIH-defined chronic GVHD occurred in a single pt at risk (cumulative incidence estimate 2.4% at 1 year, 4.7% at 2 years; Fig. 2). Four pts have reactivated EBV, with one developing PTLD (all have been treated with Rituximab). CMV reactivation was seen in 24 pts (65%), CMV disease in 4, with no deaths directly related to CMV.
In vivo T-cell depletion with r-ATG abrogates severe acute and chronic GVHD, and allows use of mismatched unrelated donors for allo-SCT in adult pts with otherwise incurable hematologic malignancies. Long-term survivors are generally free of severe chronic GVHD, with good quality of life. There does not appear to be an increased incidence of disease relapse, and non-relapse mortality is low. This approach is safe, effective, and considerably expands the donor pool for adult pts who require allo-SCT.
Reeder:Celgene: Research Funding; Millennium Pharmaceuticals Inc.: Research Funding; Novartis: Research Funding. Mesa:Incyte: Research Funding; Lilly: Research Funding; SBio: Research Funding; Astra Zeneca: Research Funding; NS Pharma: Research Funding; Celgene: Research Funding.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.