Abstract
Abstract 2069
Over the past decade there has been a shift in treating pediatric patients with RTC followed by allogeneic stem cell transplantation (alloSCT) for malignant and non-malignant diseases (Satwani/Cairo et al, BBMT 2005). Advantages of RTC over MAC include reduced acute short- and long-term late complications, reduced risk of infections, and improved survival. However, relatively little is known about the impact of RTC on the longitudinal quality of life (QOL) of these patients following alloSCT. The objective of this study was to compare the physical, emotional, and social functioning of children who received RTC versus MAC regimens prior to and after alloSCT.
Hierarchical linear modeling (HLM) was used to explore trends in the PedsQL 4.0 physical, emotional, and social functioning and select individual items of 80 children ≥ 5 years of age undergoing alloSCT between Nov. 2002 and Dec. 2008. QOL was assessed once pre-alloSCT and on days 100, 180, 365, and 730, post-alloSCT. In addition, post hoc exploratory analyses were performed to further evaluate the effect of RTC and MAC regimens on QOL outcomes. If significant between- or within-group differences were observed for any of the three sub-scales, HLM procedures were performed for each sub-scale item to identify the item(s) affected by treatment. Since post hoc analyses were exploratory no adjustments were made in the alpha level. This secondary data analysis was not powered to detect statistically significant differences. Effect size (ES) calculations were included to describe the magnitude of change in scores from baseline and were calculated using the within patient standard deviation (SD), whereas the magnitude of the difference in scores between RTC and MAC regimens were calculated using the between group SD and interpreted according to Cohen's thresholds.
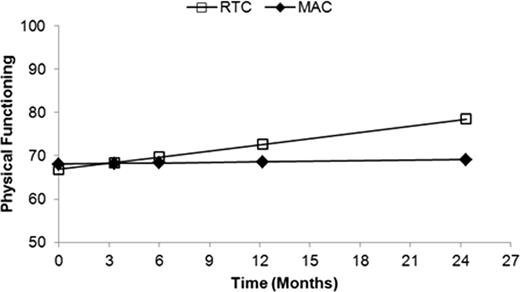
Mean age: 12.67 years; malignant/non-malignant 59%/41%; RTC/MAC 54%/46%. There was no significant difference (p = 0.87) between the baseline mean emotional functioning scores of patients treated with RTC (M = 75.90) or MAC (M = 75.30). In addition, there was no appreciable difference (p = 0.08) in the slope function between these two groups. Similarly, the baseline mean social functioning scores did not differ (p = 0.51) between groups with the RTC patients (M = 81.62) having equivalent function to MAC patients (M = 83.73). Furthermore, the rate of change over time between the two groups was not significantly different (p = 0.96). However, a significant change from baseline in overall physical functioning was estimated for RTC (M = 66.84) compared to MAC (M = 68.05) with RTC improving at a rate of 0.48 points per month (ppm)/ 5.82 points per year (ppy) and MAC improving by 0.04ppm/ 0.52ppy (t = 2.34; p = 0.02) (Figure 1). At 2-years post-alloSCT a moderate difference was estimated (ES = 0.71 SD) with RTC scoring 9.35 points higher than MAC. Post hoc analyses of physical functioning items revealed baseline impairments in lifting something heavy for both RTC (M = 55.55) and MAC (M = 56.06). However, the RTC group rapidly improved by 7.12ppm (t = 2.07; p = 0.03) with no lifting problems estimated by 6-months post-alloSCT. MAC improved by 1.27ppm, with some lifting difficulties predicted throughout the follow-up period. A large effect size difference in lifting scores was estimated at 2-years post-alloSCT with MAC scoring 6.74 SD lower than RTC. Greater improvements in fatigue scores were predicted for RTC (M = 60.11; 3.39ppm) compared with MAC (M = 65.19; 2.46ppm) (p > 0.05) with no fatigue estimated by 1-year post-alloSCT for both groups. RTC pain scores improved from baseline by 2.82ppm (M = 66.02) and 5.35ppm for MAC (M = 66.95). No difficulties with pain were estimated by 1-year for RTC and by 6-months for MAC.
Estimated change in physical functioning between RTC vs. MAC in pediatric alloSCT recipients
Estimated change in physical functioning between RTC vs. MAC in pediatric alloSCT recipients
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.