Abstract
Abstract 2140
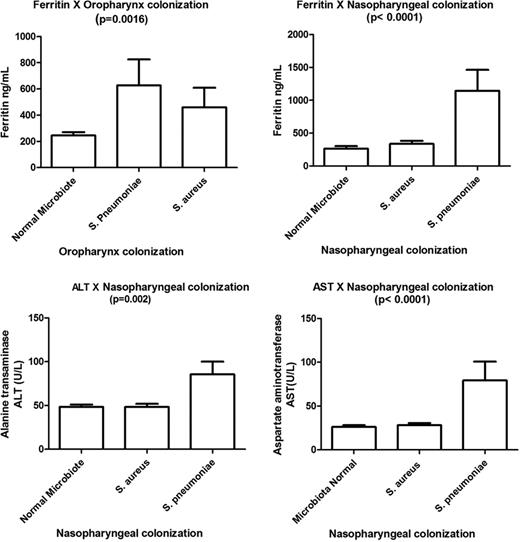
Nasopharynx and oropharynx bacterium colonization can be considered as initiation factor for local or systemic disease. The Streptococcus pneumoniae is a pathogen with epidemiological worldwide importance and it has been frequently associated with infection among SCD patients. The Staphylococcus aureus may also colonize the nasopharynx and has been associated with cause of infections in skin and soft tissue, pneumonia, sepsis, osteoarticulation. This study aimed to establish a profile of inflammation and hemolysis biomarkers of SCD individuals in association with the oropharyngeal and nasopharyngeal bacteria colonization. Patients and Methods: Biomarkers related to hemolysis and inflammation, including lipids and liver function, were determined by biochemical colorimetric reaction and also myeloperoxidase (MPO) gene polymorphisms were investigated with PCR and RFLP techniques. Medical history was obtained by patients' record. Thus, it was developed a cross-sectional study composed by 154 SCD children in a steady-state from the Bahia state, in Brazil, 68.2% (105/154) with HbSS genotype, and 31.8% (49/154) HbSC, in attendance of the outpatients clinic of the Foundation of Hematology and Hemotherapy of Bahia (HEMOBA). The study was approved by the Human research board from FIOCRUZ-BA and every official responsible signed an informed consent. Results: Nasopharynx and oropharynx colonization by S. pneumoniae was found in 14 (9.6%) SCD patients and by S. aureus in 81 (56.6%) patients, and both SCD genotypes had similar frequencies of these studied bacteria. It was not observed an increase in pneumococcal penicillin resistance. SCD patients with nasopharynx colonization by S. pneumoniae and S. aureus exhibited higher ferritin serum levels than patients with a normal microbiote respectively (p=<0.0001; p=0.0144, Mann-Whitney test). However, SCD patients with S. pneumoniae colonization had the highest ferritin serum levels. SCD patients with oropharynx colonization by S. pneumoniae exhibited the highest ferritin (p<0.0001), alanine transaminase (p=0.002) and aspartate aminotransferase (p<0.0001) serum levels when compared with SCD patients colonized by S. aureus and with normal microbiote. Evaluation of multivariate analysis models by logistic regression showed that the occurrence of infection was associated with a high number of total leukocytes (OR:3.41; CI:1.35–8.60; p=0.0092) in a model involving high levels of alpha 1-antitrypsin, antistreptolysin O, the mutant allele of myeloperoxidase gene, and nasopharynx colonization; infection was also associated in a model involving oropharynx colonization (OR:3.87; CI:1.43–10.50;p=0.008) and high leukocytes number (OR:10.13; CI:10.13–52.43; p=0.006), and high count of reticulocyte, platelets, and neutrophils. Pneumonia occurrence was associated with the HbSS genotype (OR:4.55; CI:1.56–13.31;p=0.006) in models involving oropharyngeal or nasopharyngeal colonization, and high count of reticulocyte, platelets, and neutrophils, and age less than 5 years old. Interestingly, when vaso-occlusive was analyzed, the involvement of oropharyngeal or nasopharyngeal colonization was not pivotal for this event, that was associated to high neutrophils counts (OR:11.75; CI:2.33–59.26; p=0.003) in the presence of high count of reticulocyte, platelets, leukocytes, female gender and age less than 5 years old. Conclusion: Ours result of SCD patients nasopharynx and oropharynx colonization with high ferritin serum levels may be associated with an increase of oxygen and nitrogen reactive species by bacteria presence, suggesting a pivotal role of the bacteria colonization in the modulation of hemolytic events, inflammation state, and infectious occurrence and a possible influence in the disease severity.
Hemolytic and liver function markers associated with colonization profile.
Hemolytic and liver function markers associated with colonization profile.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.