Abstract
Abstract 2612
5-Azacytidine (AZA) has proven to prolong overall survival (OS) in higher-risk MDS patients and elderly patients with WHO-defined AML and low bone marrow blast count (20–30%) compared to conventional care regimens. These exciting results have prompted us to seek the potential role of AZA on the treatment of elderly (> 60 years) patients with AML compared to best-supportive care (BSC) or intensive chemotherapy (ICT).
We have performed a retrospective analysis in 182 elderly AML patients, median age: 70y (60–84). Out of them, 67 patients from 9 Spanish centers diagnosed between Jan/07 to Feb/11 and not eligible for ICT, received 5-AZA as first line therapy by compassionate use. AZA was administered subcutaneously (75–100 mg/m2/d) for 7 days of every 28d. Patients received a median of 6 AZA cycles (1–24). For comparisons, historical cohort (N= 115) diagnosed at same period from University Hospital Reina Sofia was used. Among them, 68 patients unfit for ICT had received only BSC consisting on oral chemotherapy agents, blood product transfusions and antibiotics with granulocyte colony-stimulating factor for neutropenic infection. In this historical cohort 47 patients had received ICT consisted of induction with cytarabine (100–200 mg/m2/d by continuous infusion) for 7 days plus idarubicin (9–12 mg/m2/d) for 3 days followed by Autologous (N=9) or Allogeneic (N=4) Transplant. Outcome measures were performed according to the International Working Group criteria (AML-IWG-2006).
Clinical characteristics of patients are detailed in Table 1 . Meaningfully, patients in ICT group were significantly younger than those in BSC or AZA arms and also had significantly better ECOG scores. By contrast, patients in AZA group had significantly lower WBC and bone marrow blast count than those receiving ICT. There were not statistical differences in the presence of MDS features or gender distribution (M/F) comparing three arms. Most importantly the percentage of patients with intermediate-adverse cytogenetics was comparable between three arms.
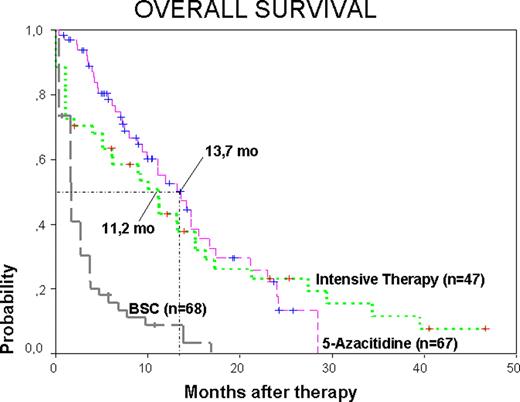
Median follow-up for surviving patients from the start of therapy was 5, 13 and 7.4 months for BSC, ICT and AZA groups respectively. The 12 months Overall Survival (OS) was 9%, 52% and 43% for BSC, ICT and AZA groups respectively. The 2y-OS was 0%, 20% and 18% for BSC, ICT and AZA groups respectively. Median OS months for BSC were 2.03 whereas for ICT and AZA groups were significantly longer: 11.2 and 13.7 respectively (Figure 1). We found statistical differences when comparing OS in BSC group with either ICT or AZA, but there was not statistical differences comparing ICT with AZA groups (p=0,75, HR=0,13; 95% CI=0,2–1,2). In multivariable Cox regression analysis, considering variables such as cytogenetic risk group, % BM Blasts and type of treatment AZA vs ICT, only high ECOG scores (p=0,01, HR=2,76; 95% CI=1,2–6) were associated with inferior survival.
These retrospective data suggest that AZA can be an effective alternative option for elderly AML patients unfit for ICT. In our experience, these patients can achieve comparable OS at 2 years than those suitable for ICT, although ECOG score remained the most independent significant variable impacting on outcome. There is a need for prospective clinical trials in order to determine the place of this approach within the growing therapeutic opportunities for elderly patients with AML.
Clinical characteristics of 182 elderly AML patients.
| . | BSC N=68 . | Intensive CT N=47 . | 5-AZA N=67 . | P . |
|---|---|---|---|---|
| Median age, y (Range) | 76 (62–89) | 65 (60–75)* | 71 (60–84)* | 0.04 <0,01* |
| Sex (M/F) | 37/31 | 30/17 | 48/19 | 0.11 |
| Median leucocyte count x109/L (range) | 17.6 (0.4–211) | 28.6 (0.8–166)* | 4.4 (0.2–17.5)* | 0.01 <0,01* |
| Median BM Blasts count (%) (range) | 47 (21–90) | 64 (24–93) | 34 (20–84) | 0.003 <0,01* |
| ECOG ≥ 2 | 60 (88%) | 7 (15%) | 45 (67%) | <0.01 <0,01* |
| Cytogenetic Risk*, N (%) | 0.67 | |||
| Intermediate | 39 (57.3) | 32 (68) | 46 (68.6) | 0.86* |
| Adverse | 12 (17.6) | 12 (25.5) | 15 (22.3) | |
| NT | 17 | 3 | 6 | |
| MDS features, N (%) | 37 (54.4) | 21 (44.6) | 34 (50.7) | 0.16 |
| Patients alive, N (%) | 10 (14.7) | 9 (19.1) | 26 (38.8) | 0.004 0,06* |
| Median,follow-up of survivors, months | 5 (0–10) | 13 (2–46) | 7.4 (1–28,3) | 0.03 0,06* |
| Median Overall Survival, months | 2,03 | 11,2* | 13,7* | <0.001 0,75* |
| OS at 1 year | 9% | 52%* | 43%* | <0.001 0,75* |
| OS at 2 years | 0% | 20%* | 18%* |
| . | BSC N=68 . | Intensive CT N=47 . | 5-AZA N=67 . | P . |
|---|---|---|---|---|
| Median age, y (Range) | 76 (62–89) | 65 (60–75)* | 71 (60–84)* | 0.04 <0,01* |
| Sex (M/F) | 37/31 | 30/17 | 48/19 | 0.11 |
| Median leucocyte count x109/L (range) | 17.6 (0.4–211) | 28.6 (0.8–166)* | 4.4 (0.2–17.5)* | 0.01 <0,01* |
| Median BM Blasts count (%) (range) | 47 (21–90) | 64 (24–93) | 34 (20–84) | 0.003 <0,01* |
| ECOG ≥ 2 | 60 (88%) | 7 (15%) | 45 (67%) | <0.01 <0,01* |
| Cytogenetic Risk*, N (%) | 0.67 | |||
| Intermediate | 39 (57.3) | 32 (68) | 46 (68.6) | 0.86* |
| Adverse | 12 (17.6) | 12 (25.5) | 15 (22.3) | |
| NT | 17 | 3 | 6 | |
| MDS features, N (%) | 37 (54.4) | 21 (44.6) | 34 (50.7) | 0.16 |
| Patients alive, N (%) | 10 (14.7) | 9 (19.1) | 26 (38.8) | 0.004 0,06* |
| Median,follow-up of survivors, months | 5 (0–10) | 13 (2–46) | 7.4 (1–28,3) | 0.03 0,06* |
| Median Overall Survival, months | 2,03 | 11,2* | 13,7* | <0.001 0,75* |
| OS at 1 year | 9% | 52%* | 43%* | <0.001 0,75* |
| OS at 2 years | 0% | 20%* | 18%* |
Kaplan Meier plot for OS in AML patients.
Off Label Use: Azacitidine in AML.
Author notes
Asterisk with author names denotes non-ASH members.