Abstract
Abstract 2757
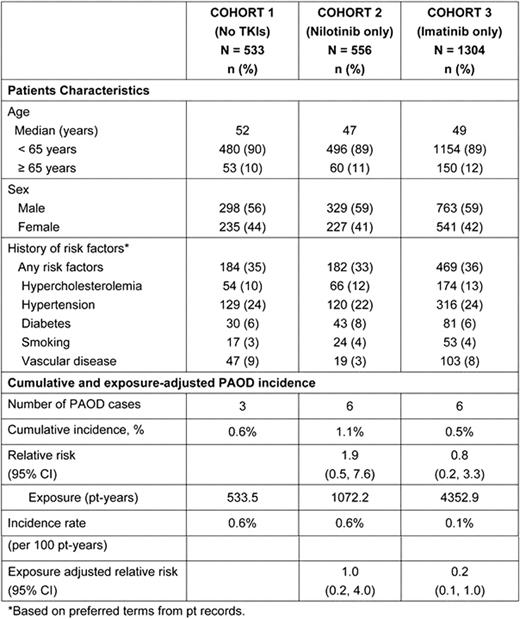
Recently there have been reports of PAOD events in pts with CML-CP treated with tyrosine kinase inhibitors (TKI). Although asymptomatic PAOD is common, occurring in 12–20% of adults (55–70 years of age), the incidence of PAOD in pts with CML is unknown. Risk factors for PAOD include hypercholesterolemia, hypertension, diabetes, smoking, and vascular disease. It remains to be determined if PAOD may be related to CML and/or TKIs. These considerations are important as atherosclerotic disease has been observed with other pt populations (HIV and hemophilia) with improved survival similar to CML due to effective treatments. To investigate the association of PAOD in CML pts a retrospective cohort analysis was conducted with the objective of comparing TKI treated pts to a comparator arm of no TKI therapy. Methods: This analysis was based on a database of pooled randomized, multi-center, clinical trial data from ENESTnd, TOPS, and IRIS in pts with newly-diagnosed CML-CP. From this database (n = 2393), 3 cohorts of pts were generated: Cohort 1–No TKI exposure (IFN+Ara-C only, n = 533), Cohort 2–Nilotinib only (300 and 400 mg BID, n = 556) and Cohort 3–Imatinib only (400 mg QD or BID, n = 1304). Exclusion criteria for cardiovascular disease varied across cohorts and pts with risk factors for PAOD were not excluded in any cohorts. The case definition for PAOD included atherosclerotic and thrombotic events, excluding the functional (vasoreactive), embolic, or aneurysmal disorders, in the arteries of lower and upper extremities according to ACC/AHA guidelines. Events indicative of PAOD were represented by a group of broad terms including: arterial disorder, arteriosclerosis, peripheral ischaemia, arterial insufficiency, arteriosclerosis obliterans, peripheral vascular disorder, arterial occlusive disease, femoral arterial stenosis, arterial stenosis, femoral artery occlusion, peripheral artery angioplasty, arterial stenosis limb, intermittent claudication, peripheral revascularization, arterial thrombosis limb, peripheral arterial occlusive disease, and poor peripheral circulation. The cumulative incidence of PAOD cases reported represents the crude rate without accounting for duration of exposure; exposure adjusted incidence rate was also provided since the duration of therapy differed substantially among cohorts. Relative risks (RR) with 95% confidence intervals (CI) are presented for Cohorts 2 (nilotinib only) and 3 (imatinib only) compared with Cohort 1 (no TKIs). Results: As shown in the table, when using Cohort 1 (no TKIs) as the control for TKI therapies the RR for Cohort 2 (nilotinib only) was 1.9 (95% CI 0.5, 7.6) and the RR for Cohort 3 (imatinib only) was 0.8 (95% CI 0.2, 3.3). When accounting for exposure using pt-years, the exposure adjusted RR was 1.0 (95% CI 0.2, 4.0) for Cohort 2 (nilotinib only), and 0.2 (95% CI 0.1, 1.0) for Cohort 3 (imatinib only). The CIs for these RRs overlap 1.0 suggesting no significant increased risk. Conclusions: Based on the large cohort of pts in this analysis, the results demonstrate a low incidence of PAOD cases for pts on either nilotinib or imatinib. In comparison with the no-TKI control, the risk and causality of PAOD due to nilotinib or imatinib could not be established with current available data. However, caution should be exercised when interpreting retrospective comparisons and further investigation is required to better understand whether PAOD events are increased in CML pts treated with TKIs.
Giles:Novartis: Consultancy, Honoraria, Research Funding. Mauro:Novartis: Research Funding; Bristol Myers Squibb: Research Funding; Ariad: Research Funding. Hong:Novartis: Employment. Ortmann:Novartis: Employment. Woodman:Novartis: Employment, Equity Ownership. LeCoutre:Bristol Myers Squibb: Honoraria; Novartis: Honoraria, Research Funding, Speakers Bureau. Saglio:Bristol Myers Squipp: Consultancy, Speakers Bureau; Novartis Pharmaceutical: Consultancy, Speakers Bureau; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.