Abstract
Abstract 2791
Most MDS patients require chronic red blood cell (RBC) transfusion. Despite the immediate benefit of transfusion, transfusion dependence in MDS is a negative prognostic factor for overall survival. It has been suggested that transfusional iron overload, which is linked to toxicity through oxidative stress, contributes to poorer disease outcome and even to the progression of MDS to acute leukaemia. Alternatively, transfusion requirements may merely reflect disease severity in MDS and hence inferior disease outcome. To date, the exact relationship between transfusion, disease severity and outcome remains unclear. Nevertheless, aside from dependency, there are other essential aspects in transfusion medicine such as transfusion rate and patterns. We therefore examined the transfusion history of MDS patients to explore possible pathophysiological and prognostic values of these parameters.
We performed retrospective single institution study of 40 consecutive chronically transfused patients between May 1998 and May 2011in the MDS program at the Odette Cancer Centre of Sunnybrook Hospital, Ontario, Canada. Median follow-up was 60 months. Median age was 72 years (range 28–88). 25 patients were male. WHO diagnostic categories were: 5q=2, CMML1=2, MDS/MPD=2, RA=2, RARS=1, RCMD=9, RCMD-RS=4, T-MDS=1, Unclassified=4, CMML2=2, RAEB1=2, RAEB2=4, AML=5. IPSS risk groups were: No score=5, low-risk=6, int-1=15, int-2=4, high-risk=10. 11 patients received iron chelation therapy. 20 patients received active treatment beyond transfusions.
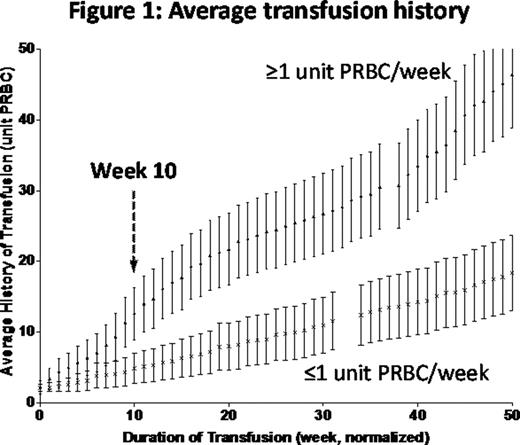
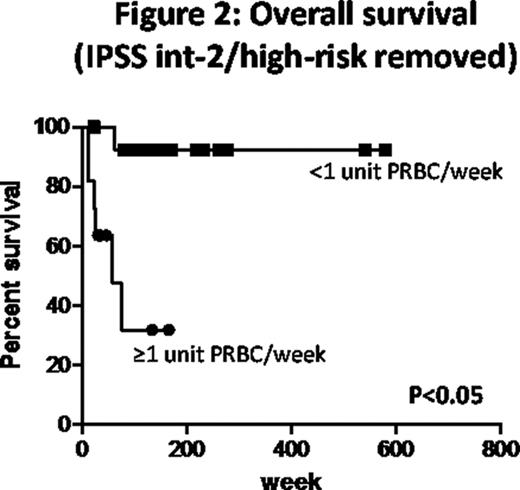
Overall survival (OS) at 100 weeks was 54.1%. IPSS category (low/int-1 vs. int-2/high-risk) was a significant predictor of OS according to the Cox proportional-hazards regression (P<0.005, HR=7.39, median survival = 49 weeks for int-2/high-risk patients with 33.3% survival at 100 weeks, 69.4% survival at 100 weeks for low-risk/int-1 patients). To examine the prognostic importance of initial transfusion rate (ITR) in MDS we analyzed the total number of PRBC units transfused in the first 10 weeks after each patient became transfusion dependent to derive the ITR (unit PRBC/week, u/wk). In this way the patients were separated into two groups: low ITR (<1 u/wk, N=24, 73.2% survival at 100 weeks) and high ITR (≥1 u/wk, N=13, median survival at 58 weeks and 27% survival at 100 weeks). At week 10, we observed a divergence of the average transfusion history curves between the low and high ITR groups (Figure 1). Multivariate analysis identified ITR (P<0.0001, HR=18.6), IPSS (P<0.005, HR=15.2) and iron chelation (P<0.05, HR=11.4) as statistically significant predictors of overall survival. When analysis was limited to only those patients with IPSS low/int-1 risk categories (Figure 2), Cox regression revealed ITR as the sole predictor of OS (N=14 for low ITR group, 65.5% survival at 100 weeks; N=11 for the high ITR group, median survival at 24 weeks; P<0.05, HR=78.1).
To examine possible dose-response trend related to ITR, the patients were re-organized into 3 groups: <0.5 u/wk (N=10, 90% survival at 100 weeks), ≥0.5 to <1 u/wk (N=14, 59.2% survival at 100 weeks) and ≥1 u/wk (N=13, median survival at 58 weeks and 27% survival at 100 weeks). A statistically significant trend was identified using the Logrank test for trend (P<0.005). Subsequent multivariate analysis identified ITR (P<0.0001, HR=10.5), IPSS (P<0.001, HR=18.7) and iron chelation (P<0.05, HR=23.0) as predictors of OS. After patients with IPSS from int-2/high-risk were removed from the analysis, ITR is the only predictor of OS (P<0.05, HR=48.8).
The initial rate of RBC transfusion after onset of transfusion dependence is a powerful predictor of outcome in MDS and appears to be independent of WHO category or IPSS. Patients with high transfusion requirement (more than 1 u/wk) can be rapidly identified after they become transfusion dependent (as soon as 10 weeks). Although the pathophysiological basis of the link between ITR and disease outcome remains to be determined, and there is a need to validate this observation in an independent cohort, this parameter can be included in prognostic scoring systems for MDS. Patients with high ITR are likely to require additional treatments such as bone marrow transplantation or experimental therapies as soon as they are identified.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.