Abstract
The life expectancy of patients with myeloproliferative neoplasms (MPNs) is overall shorter than that of the general population. This is considered true for patients with polycythemia vera and primary myelofibrosis. A recent study by our group showed an inferior relative survival also for patients with essential thrombocythemia. Relative survival of MPN patients improved over the last decades but an excess mortality was observed among patients with all subtypes also during recent calendar periods. To elucidate the underlying causes of this excess mortality, we assessed the causes of death using a competing risk model in a large cohort of patients diagnosed with MPNs in Sweden 1973–2005 and compared the findings to those of matched controls.
Patients were identified from the Swedish Cancer Registry and through our national MPN network. Matched controls without a hematological malignancy were identified through the Swedish Register of Total Population. Causes of death were identified using the Swedish Cause of Death Registry with follow-up until 2007. Cox regression was used to identify hazard ratios (HRs) with 95% confidence intervals (CIs) of dying from six different categories of death; infection, solid tumor, hematological malignancy, cardiovascular disease, cerebrovascular disease and other conditions. A competing risk analysis based on the Cox proportional hazards model was performed and results presented as stacked cumulative incidence plots.
We identified 9,563 MPN patients and their 37,643 controls. Forty-seven per cent of patients were males and the median age at diagnosis was 70 years. The distribution of cause specific deaths was similar for all MPN subtypes. The following results represent all MPN subtypes taken together. As expected, the probability of dying from any cause during the first 10 years after diagnosis was higher for cases compared to controls. For example, in MPN patients aged 70–79 at diagnosis the HR of dying from infection was 2.8 (CI 2.3–3.3), solid tumor HR=1.2 (1.1–1.4), hematological malignancy HR=∞, cardiovascular disease HR=1.5 (1.4–1.7), cerebrovascular disease HR=1.5 (1.3–1.8) and other disorders HR=2.1 (2.0–2.3). The probability of dying was higher in older persons and this age related effect was more pronounced in cases than controls. The overall mortality was very low in the youngest age group, so whilst in relative terms the risk of dying is far greater in the cases than the controls, in absolute terms the actual number of patients dying is quite small. For example the HR of dying from infections was 22.6 (8.4–60.8) and from cardiovascular disease HR=4.4 (2.8–7.0) in cases diagnosed between ages 18–49 years.
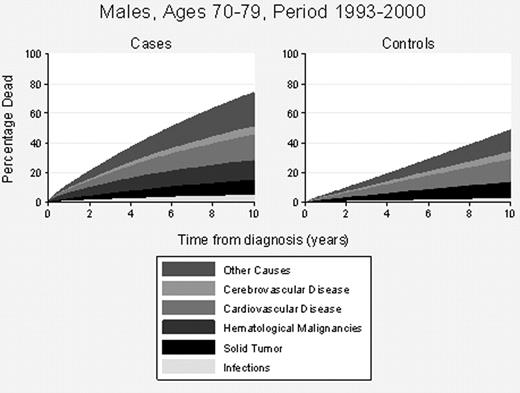
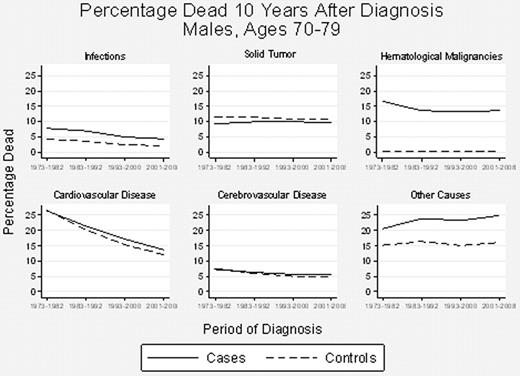
In the competing risk model, studying male patients diagnosed between ages 70–79 during the calendar period 1993–2000 the overall probability of dying was 74% compared to 49% in controls within 10 years from diagnosis (Figure 1). The distribution of probabilities of cause specific death for cases and controls (within parenthesis) were infection 4.9% (2.4 %), solid tumors 9.9% (10.9%), hematological malignancy 13.4% (0.2%), cardiovascular disease 17.2% (15.3%), cerebrovascular disease 5.6% (5.0%) and other disorders 23.2% (15.1%) (Figure 1). The 10-year mortality rates decreased with calendar period for both cases and controls, both genders and for all age groups. The probability of dying from hematological malignancy in MPN patients remained the same over all calendar periods. The risk of cardiovascular death showed the largest decrease over time; however the decrease in risk was similar for both cases and controls (Figure 2).
MPN patients in all subgroups had a higher probability of dying during the first 10 years after diagnosis compared to controls, mainly explained by death from a hematological malignancy. The major decrease in cardiovascular death in patients over the calendar periods is probability the main contributing factor to the improvement in 10-year survival. However, an almost identical trend was observed among controls suggesting a general improvement in the management of cardiovascular disease. Taken together the reason for the observed improvement in survival in MPN patients over time is probably multifactorial and is not only attributed to the management of the underlying hematological disorder per se. Studies elucidating contributing factors are ongoing.
Björkholm:Shire: Research Funding.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.