Abstract
Abstract 4146
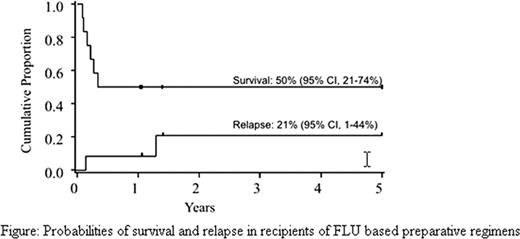
Fanconi anemia (FA) patients with acute leukemia or advanced myelodysplastic syndrome (MDS with ≥ 5% blasts) have a poor prognosis and hematopoietic cell transplantation (HCT) experience is limited. We report on the outcomes of 21 patients with FA and acute myeloid leukemia (AML, n=16), acute lymphocytic leukemia (ALL, n=2) or advanced MDS (n=3) who underwent allogeneic HCT at the University of Minnesota from 1988–2009. Five patients had biallelic BRCA2 mutations. Only 2 of 7 patients who received chemotherapy before HCT achieved remission both of whom had biallelic BRCA-2 mutations and T-cell ALL. Median age was 15.5 (range 1.1–48.5) years. Median age for BRCA2 patients was substantially lower at 1.9 (range 1.4–6.6) years. Patients received cyclophosphamide, antithymocyte globulin and either single fraction total body irradiation (n=15) or busulfan (n=6), with (n=11) or without (n=10) fludarabine (FLU) followed by HLA-matched sibling (n=3) or alternative (n=18) donor stem cells consisting of bone marrow (BM, n=14), single (n=4) or double (n=3) umbilical cord blood (UCB). Graft-versus-host disease (GVHD) prophylaxis consisted of cyclosporine A and methylprednisolone. Probability of neutrophil engraftment was 75% without FLU and 100% with FLU based regimens. Probability of acute GVHD was 19%. For the entire cohort, probability of survival at 1 year was 43%. A higher rate of survival was observed in the 11 patients who received a FLU based regimens (50%; figure) and in the 5 patients with BRCA2 mutations (60%). Probability of relapse was 21% in these 11 patients.
These data suggest that HCT with a FLU based preparative regimen offers potential curative therapy for FA patients with acute leukemia or advanced MDS. Except perhaps for BRCA-2 patients with T cell ALL, there is no clear role for chemotherapy prior to HCT in FA patients with AML or MDS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.