Abstract
Abstract 4610
Infections are a major cause of morbidity and mortality in patients with chronic lymphocytic leukemia (CLL). Up to 50% of CLL patients develop infectious complications, and 30–50% of all deaths in CLL patients are attributed to infections. Despite these data, the available research on infectious complications in CLL is primarily limited to patients participating in clinical trials of chemotherapy, obscuring the distinction between the risk of infection due to the disease’s natural history relative to the risk associated with therapy related immune suppression.
The Mayo Clinic Rochester (MCR), a tertiary referral center in rural southeastern Minnesota, is also the primary hematology center for southeastern Minnesota, northern Iowa, and western Wisconsin. There are no metropolitan areas or hematology specialty centers within a ∼50 mile radius. To explore the natural history of infection in a community-based cohort of CLL patients, we used the Mayo Clinic CLL database to identify all patients with newly diagnosed CLL who resided within 50 miles of MCR and diagnosed between January, 1999 and December, 2009. The comparison cohort consisted of 689 adult patients who also resided within 50 miles of MCR who were seen for a general medical examination between September, 2002 and December, 2009 and who were enrolled as controls in a case-control study of non-Hodgkin lymphoma. All hospitalizations at MCR among both cohorts were audited to document hospitalization with infection and cross-referenced with the Mayo Clinic infection database, which includes all culture results obtained from hospitalized MCR patients. Serologies and viral assays were also reviewed. Patients whose cultures were negative but who were given a clinical diagnosis of infection (e.g. pneumonia) and who were treated with a full course of antibiotic therapy were considered to have a culture negative infection.
In May 2010, there were 2022 CLL patients in the Mayo Clinic CLL Database diagnosed between 1999 and 2009. Of these, 174 (9%) were local CLL patients residing within 50 miles of MCR. Median age at diagnosis for these non-referred CLL patients was 69 years (range 27–97). Most had early stage disease (60% stage 0; 32% stage I-II). On prognostic evaluation, 121 (75%) patients were CD38 negative, 66 (61%) ZAP-70 negative, 47 (50%) IGHV mutated, and 56 (62%) had either no abnormality or 13q14- as a sole abnormality on FISH analysis. 64 (37%) patients progressed to require treatment for CLL during follow-up.
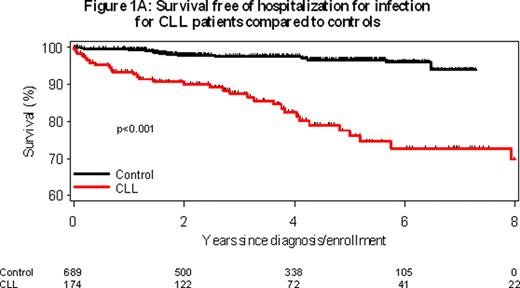
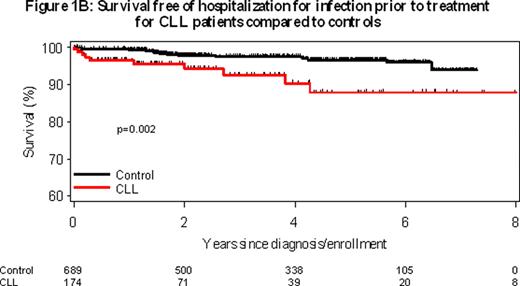
After median follow-up of 4.0 years (range 0–11), 32 (18.4%) CLL patients were hospitalized with infection at least once as compared to 20/689 (2.9%) individuals in the control cohort (odds ratio=7.5; p<0.0001) Figure 1A. Even prior to receiving treatment for CLL, the rate of hospitalization for infection remained higher than the control cohort (p=0.002; Figure 1B). The 32 CLL patients hospitalized with infection were admitted with infection a total of 89 times (median 1 hospitalization for infection per patient). A specific infectious organism was identified by cultures or serologies in 60 (63%) of the 89 infections in CLL cases and 10/27 (37%) infections among controls. Hospitalization for an opportunistic infection (e.g. cytomegalovirus, cryptococcus, filamentous fungi, mycobacteria, Pneumocystis) occurred in 5/174 (3%) CLL patients during follow-up compared to 0/689 controls (p<0.001).
Finally, we performed a pooled multivariable analysis of all patients (n=863) to identify factors (age, sex, CLL diagnosis, CLL treatment) associated with infection risk. Most factors were independently associated with hospitalization for infection [Age (per year, OR=1.03, p=0.02), sex (male, OR=4.0, p<0.001), diagnosis of CLL (OR=2.1, p=0.09), and treatment for CLL (OR=5.9, p<0.001)]. In univariate analysis of CLL patients [sex (OR=4.2, p=0.01), higher Rai stage (p=0.046), unfavorable (del 17p13; del 11q23) FISH [OR=4.6, p=0.02] and unmutated IGHV [OR=2.8, p=0.07]) were associated with risk of infection.
In this cohort study, patients with newly diagnosed CLL had a 7.5-fold risk of hospitalization for infection relative to the control cohort. After 4 year follow-up, ∼1 in 5 CLL patients required hospitalization for infection. Although CLL treatment was a substantial risk factor for infection, the risk of infection among untreated patients remained higher than controls.
Kay:Biothera: Research Funding; Clegene: Research Funding; Cephalon: Research Funding; Genentech: Research Funding; Glaxo Smith Kline: Research Funding; Hospira: Research Funding; Novartis: Research Funding; Supergen: Research Funding; Calistoga: Membership on an entity’s Board of Directors or advisory committees; Celgene: Membership on an entity’s Board of Directors or advisory committees; Emergent Biosolutions (Formerly Trubion): Membership on an entity’s Board of Directors or advisory committees. Zent:GlaxoSmithKline: Research Funding; Genentech: Research Funding; Genzyme: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.