Abstract
Abstract 4774
The Fall of the Erythrocyte Sedimentation Rate, Ashley J. Archambault, MLS(ASCP), Gyorgy Abel, MD, PhD, John Gawoski, MD, Tim Skelton, MD, PhD, Charles Arkin, MD, Department of Laboratory Medicine, Lahey Clinic Medical Center, Burlington MA
The Erythrocyte Sedimentation Rate (ESR) is widely used to indicate the presence of active inflammation, particularly in rheumatic and infectious disorders. It has long been a mainstay in diagnostic protocols, as well as being a standard in the work-up of temporal arteritis. However, despite its entrenchment in the minds of many physicians, an increasing number of medical professionals believe that the ESR should be eliminated since its results are often misleading and too nonspecific. Moreover other indicators of inflammation such as the C-reactive protein (CRP) and fibrinogen are now readily available to provide more reliable information. The ESR is also costly, labor intensive, and hazardous to laboratory personnel.
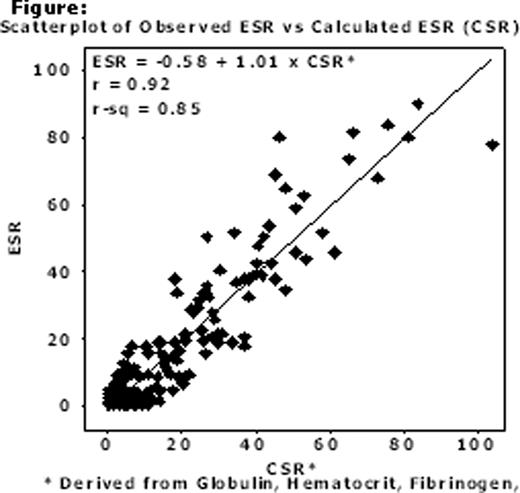
Based on the above, Lahey Clinic Medical Center eliminated ESR testing in April of 2010. To accomplish this, an initial informational campaign was launched among the Lahey Clinic medical staff. Literature was distributed and face-to-face meetings were conducted with the most frequent users of the test. Details of the ESR's limitations and the suitability of its replacement by the CRP were emphasized. To strengthen the contention that ESRs are not essential to our institution, two in-house studies were performed: Study 1 reviewed 6 months of patient data from 2008 in order to evaluate cases where the CRP was negative and the ESR was positive. Study 2 used multiple regression analysis to show that ESR values could be calculated from, and presumably replaced by, other clinical data.
Results of 4858 Paired CRP/ESR Tests over 6 Months in 2008
| . | ESR . | ||||
|---|---|---|---|---|---|
| CRP | ≤20 | >20 ≤50 | >50 | TOTAL | |
| ≤5 | 1830 | 304 | 17 | 2151 | |
| >5 ≤10 | 818 | 326 | 56 | 1200 | |
| >10 | 446 | 614 | 447 | 1507 | |
| TOTAL | 3094 | 1244 | 520 | 4858 | |
| . | ESR . | ||||
|---|---|---|---|---|---|
| CRP | ≤20 | >20 ≤50 | >50 | TOTAL | |
| ≤5 | 1830 | 304 | 17 | 2151 | |
| >5 ≤10 | 818 | 326 | 56 | 1200 | |
| >10 | 446 | 614 | 447 | 1507 | |
| TOTAL | 3094 | 1244 | 520 | 4858 | |
In late 2009 a memo went out to our physicians giving three months notice of the ESR's discontinuation and recommending use of the CRP in its place. During this period, reminders of the approaching deadline were appended to all ESR results. For the Departments of Rheumatology and Infectious Diseases, an additional three months were granted during which time calculated ESR, fibrinogen, globulin, and hematocrit values were reported for every ESR ordered.
In comparison to Study 1, the same six month period in 2011 shows a fall of 10,802 ESRs, a gain of 5,669 CRPs, and a drop in utilization of about 5,000 tests or 10,000 per year. These numbers suggest that CRPs replaced the unpaired ESRs and the utilization drop was due primarily to deletion of ESRs from paired orders.
Over sixteen months of post ESR testing, the laboratory received only four inquiries from the medical staff: a complaint that a CRP did not automatically replace an ESR order; a request for supportive literature; and two requests for ESR values that were needed to satisfy standard treatment protocols. The latter were provided with calculated ESRs.
In summary, ESR elimination occurred smoothly and with minimal incident. Sixteen months of experience have yielded no negative clinical effects but have produced the perceived benefits of utilization reduction, more available technologist time, less bio-hazard exposure, and elimination of an obsolete test.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.