Abstract
Generation of patient-specific induced pluripotent cells (iPSCs) holds great promise for regenerative medicine. Epstein-Barr virus immortalized lymphoblastoid B-cell lines (LCLs) can be generated from a minimal amount of blood and are banked worldwide as cellular reference material for immunologic or genetic analysis of pedigreed study populations. We report the generation of iPSCs from 2 LCLs (LCL-iPSCs) via a feeder-free episomal method using a cocktail of transcription factors and small molecules. LCL-derived iPSCs exhibited normal karyotype, expressed pluripotency markers, lost oriP/EBNA-1 episomal vectors, generated teratomas, retained donor identity, and differentiated in vitro into hematopoietic, cardiac, neural, and hepatocyte-like lineages. Significantly, although the parental LCLs express viral EBNA-1 and other Epstein-Barr virus latency-related elements for their survival, their presence was not detectable in LCL-iPSCs. Thus, reprogramming LCLs could offer an unlimited source for patient-specific iPSCs.
Introduction
Patient-specific induced pluripotent stem cells (iPSCs) can serve as useful models for understanding the etiology of disease and facilitating the development of novel therapeutic interventions.1 B cells represent a larger fraction of the peripheral blood mononuclear cell population (∼ 20%) and can be transformed in vitro by Epstein-Barr virus (EBV) to generate lymphoblastoid cell lines (LCLs) using as little as 0.5 mL blood,2 creating an unlimited proliferative source of cells for reprogramming trials. LCLs are a precious resource for immunologic, epidemiologic, and rare disease studies. A number of facilities manage collections of LCLs available internationally to researchers.2 Thus, generating iPSCs from LCLs offers the advantage of working with minimal amounts of blood from living donors as well as frozen LCL collections banked worldwide.
The capability to reprogram terminally differentiated cells depends on the inherent physiologic plasticity of the cell type. B lymphocytes can transdifferentiate to macrophages3,4 or hematopoietic precursor cells (HPCs) after down-regulation of Pax5 expression.4 Murine B cells have been reprogrammed to iPSCs via viral transduction of reprogramming factors with5 and without Pax5 inhibition.6 Generating iPSCs via nonviral, nonintegrating methods is appealing to generate clinically useful iPSCs. Recently, iPSCs have been generated by delivering the reprogramming factors via oriP/EBNA-1–based plasmids in fibroblasts and peripheral blood CD34+ cells.7,8 The inherent plasticity of B cells, their receptivity to oriP/EBNA-1 plasmids, ease of generating LCLs, and availability of banked LCL collections inspired our efforts to reprogram LCLs using oriP/EBNA-1–based vectors.
LCL-derived iPSCs (LCL-iPSCs) demonstrated the characteristics of pluripotent stem cells, a normal karyotype, the genetic identity, and IgGH signature of the parental LCLs and lost expression of the episomal reprogramming genes as well as viral genes, leading to self-sustained LCL-iPSCs essentially free of exogenous reprogramming and viral elements.
Methods
Detailed methods are included in supplemental Methods (available on the Blood Web site; see the Supplemental Materials link at the top of the online article). All animal experiments were conducted according to relevant national and international guidelines under the approval of the Cellular Dynamics International Animal Care and Use Committee.
Briefly, LCLs obtained from Coriell Cell Repository (GM02254 and GM22649) were transfected using oriP/EBNA-1–based vectors9,10 and then placed on Matrigel-coated plates (BD Biosciences) in reprogramming medium11 for 2 to 3 weeks followed by TeSR-2 (StemCell Technologies) for an additional 2 weeks. After handpicking, the iPSC-like colonies were propagated with TeSR-2 on Matrigel-coated plates. Characterization of 4 LCL-iPSCs was performed by flow cytometry, RT-PCR, and teratoma analysis.9 In vitro differentiations were performed to neural, hematopoietic, cardiac, and hepatocyte-like lineages. The presence of EBV was assessed by RT-PCR, immunohistochemistry, and quantitative PCR (Department of Pathology, University of North Carolina). G-banding of LCL-iPSCs (WiCell Research Institute) and IgGH receptor rearrangement analysis (Hematologics) on parental and LCL-iPSCs were performed, and short tandem repeat analysis confirmed genetic identity to the parental LCLs (Cell Line Genetics).
Results and discussion
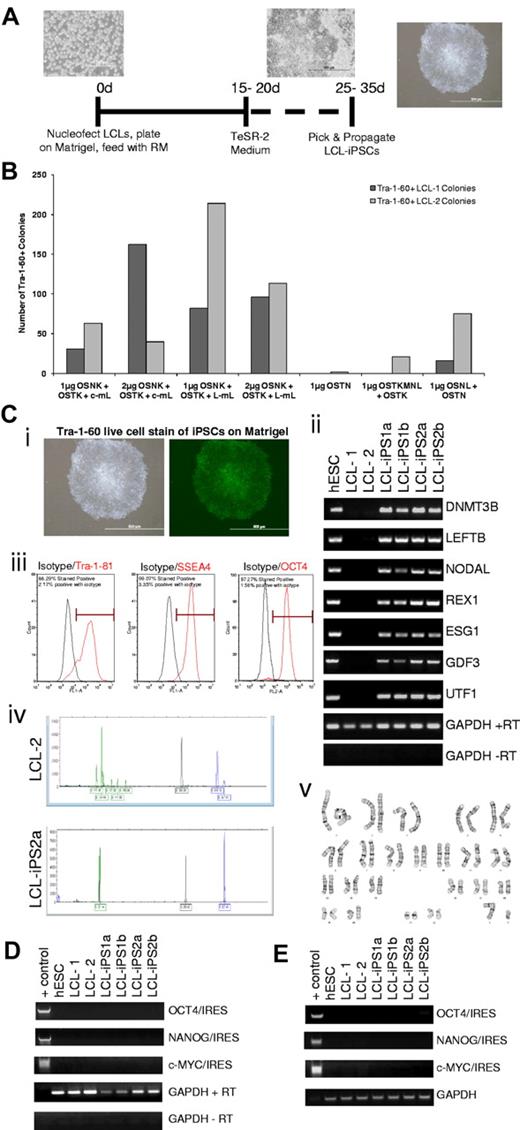
LCLs were reprogrammed to iPSCs via a single transfection of oriP/EBNA-1 plasmids encoding reprogramming genes under feeder-free conditions previously described.11 LCLs were placed on Matrigel-coated plates after transfection and cultured with reprogramming medium until adherent colonies were visible (Figure 1A) and then transitioned to TeSR-2. After approximately 2 weeks of culturing in TeSR-2, the pluripotent status of the colonies was assessed by live-cell staining of Tra-1–60 (Figure 1Ci); 2% to 23% of total adherent colonies by day 35 were confirmed to be iPSCs by Tra-1–60 staining. Various combinations of reprogramming plasmids were capable of reprogramming LCLs (Figure 1B; supplemental Table 1); a minimal combination of OCT3/4, SOX2, NANOG, and SV40-T antigen was sufficient to reprogram LCLs. This method is more efficient than the average efficiency of viral reprogramming terminally differentiated murine B cells,6 but not as efficient as episomal reprogramming of human fibroblasts or cord blood11 (supplemental Table 2). The amenability of LCLs to episomal reprogramming could be dependent on the broad rearrangement of chromatin architecture orchestrated by EBNA-1 to create an “open” chromatin state during the immortalization of B cells by EBV.12 These pleotrophic effects of EBNA-1 and expression of other viral proteins may favor reprogramming of LCLs compared with primary cells.13
Derivation and characterization of LCL-iPSCs. (A) The scheme for reprogramming human LCLs. Morphology of an LCL culture, cells during reprogramming, and LCL-iPSC colonies. Images were captured using original magnification ×40, ×20, and ×10, respectively. (B) The graph illustrates the average number of Tra-1–60-positive colonies formed after nucleofection of LCL-1 and LCL-2 with various combinations of reprogramming factors at day 40 after nucleofection. The abbreviations used for the reprogramming factors are as follows: O indicates OCT4; S, SOX2; N, NANOG; K, KLF4; c-m, c-MYC; L-m, L-MYC; T, SV40 large T antigen; and L, LIN28. Construction of the plasmids and the emergence of the colonies are described in the Supplemental data. (C) Characterization of LCL-iPSC lines. (i) Brightfield (left panel) and Tra-1–60 staining (right panel) of a representative LCL-derived iPSC line (LCL-iPS2a) confirms uniform expression of the pluripotent surface marker, Tra-1–60. Images were taken using original magnification ×10. (ii) RT-PCR analysis of H1 (hESC line), LCL-1, LCL-2, and 2 representative LCL-iPS clones from each donor lines for expression of hES cell-marker genes DNMT3B, LEFTB, NODAL, REX1, ESG1, GDF3, and UTF1. GAPDH was used as positive loading control for each sample, and cDNA made in the absence of reverse transcriptase (no RT) was used to verify that genomic DNA did not contaminate the RNA samples. (iii) Flow cytometric analysis of hESC pluripotency markers Tra-1–81 (left panel: red line indicates Tra-1–81; and black line, isotype control), SSEA-4 (middle panel: red line indicates SSEA4; and black line, isotype control), and OCT4 (right panel: red line indicates OCT4; and black line, isotype control) of a representative LCL-derived iPS line, LCL-iPS1b. (iv) Each B-cell has a respective single productive immunoglobulin gene rearrangement that is unique in both length and sequence. PCR assays with specific primers for the joining region and all 3 of the conserved framework regions (FR1, FR2, and FR3) were used to amplify immunoglobulin heavy chain (IgGH) gene rearrangements according to the BIOMED-2 Concerted Action protocol. DNA from a normal or polyclonal B-cell population produces a bell-shaped curve of amplicon products (Gaussian distribution), whereas clonal rearrangements are identified as prominent, single-sized products by capillary electrophoresis and GeneScanning. (v) Karyotype analysis of each iPSC line was performed after 11 passages and found to be normal (a representative image of LCL-iPS2b is shown). (D) RT-PCR analysis of RNA from LCL-iPSCs for the expression of reprogramming vector genes at passage 25. Forward primers for 3 reprogramming genes of interest (OCT4, NANOG, and c-MYC) and reverse primers for internal ribosome entry site 2 were used. GAPDH was used as a positive loading control for each sample, and cDNA made in the absence of reverse transcriptase (no RT) was used to verify that genomic DNA did not contaminate the RNA samples. A reprogramming vector was included as a positive control for each PCR reaction (+ control). (E) PCR analysis of genomic DNA confirms no integration of the transgenes in LCL-iPSCs at passage 25. Forward primers for 3 reprogramming genes of interest (OCT4, NANOG, and c-MYC) and reverse primers for the internal ribosome entry site were used. GAPDH was used as a positive loading control for each sample, and a reprogramming vector was included as a positive control for each PCR reaction (+ control). All images were captured on a Olympus 1×71 microscope equipped with a Olympus DP70 camera and DP Controller Version 3 software.
Derivation and characterization of LCL-iPSCs. (A) The scheme for reprogramming human LCLs. Morphology of an LCL culture, cells during reprogramming, and LCL-iPSC colonies. Images were captured using original magnification ×40, ×20, and ×10, respectively. (B) The graph illustrates the average number of Tra-1–60-positive colonies formed after nucleofection of LCL-1 and LCL-2 with various combinations of reprogramming factors at day 40 after nucleofection. The abbreviations used for the reprogramming factors are as follows: O indicates OCT4; S, SOX2; N, NANOG; K, KLF4; c-m, c-MYC; L-m, L-MYC; T, SV40 large T antigen; and L, LIN28. Construction of the plasmids and the emergence of the colonies are described in the Supplemental data. (C) Characterization of LCL-iPSC lines. (i) Brightfield (left panel) and Tra-1–60 staining (right panel) of a representative LCL-derived iPSC line (LCL-iPS2a) confirms uniform expression of the pluripotent surface marker, Tra-1–60. Images were taken using original magnification ×10. (ii) RT-PCR analysis of H1 (hESC line), LCL-1, LCL-2, and 2 representative LCL-iPS clones from each donor lines for expression of hES cell-marker genes DNMT3B, LEFTB, NODAL, REX1, ESG1, GDF3, and UTF1. GAPDH was used as positive loading control for each sample, and cDNA made in the absence of reverse transcriptase (no RT) was used to verify that genomic DNA did not contaminate the RNA samples. (iii) Flow cytometric analysis of hESC pluripotency markers Tra-1–81 (left panel: red line indicates Tra-1–81; and black line, isotype control), SSEA-4 (middle panel: red line indicates SSEA4; and black line, isotype control), and OCT4 (right panel: red line indicates OCT4; and black line, isotype control) of a representative LCL-derived iPS line, LCL-iPS1b. (iv) Each B-cell has a respective single productive immunoglobulin gene rearrangement that is unique in both length and sequence. PCR assays with specific primers for the joining region and all 3 of the conserved framework regions (FR1, FR2, and FR3) were used to amplify immunoglobulin heavy chain (IgGH) gene rearrangements according to the BIOMED-2 Concerted Action protocol. DNA from a normal or polyclonal B-cell population produces a bell-shaped curve of amplicon products (Gaussian distribution), whereas clonal rearrangements are identified as prominent, single-sized products by capillary electrophoresis and GeneScanning. (v) Karyotype analysis of each iPSC line was performed after 11 passages and found to be normal (a representative image of LCL-iPS2b is shown). (D) RT-PCR analysis of RNA from LCL-iPSCs for the expression of reprogramming vector genes at passage 25. Forward primers for 3 reprogramming genes of interest (OCT4, NANOG, and c-MYC) and reverse primers for internal ribosome entry site 2 were used. GAPDH was used as a positive loading control for each sample, and cDNA made in the absence of reverse transcriptase (no RT) was used to verify that genomic DNA did not contaminate the RNA samples. A reprogramming vector was included as a positive control for each PCR reaction (+ control). (E) PCR analysis of genomic DNA confirms no integration of the transgenes in LCL-iPSCs at passage 25. Forward primers for 3 reprogramming genes of interest (OCT4, NANOG, and c-MYC) and reverse primers for the internal ribosome entry site were used. GAPDH was used as a positive loading control for each sample, and a reprogramming vector was included as a positive control for each PCR reaction (+ control). All images were captured on a Olympus 1×71 microscope equipped with a Olympus DP70 camera and DP Controller Version 3 software.
Extensive characterization was performed on 2 clones derived from LCL-1 (LCL-iPS1a and LCL-iPS1b), and 2 from LCL-2 (LCL-iPS2a and LCL-iPS2b). These clones had more than or equal to 90% expression of SSEA-4, Tra-1–81, and OCT3/4 (Figure 1Ciii) demonstrated by flow cytometry. LCL-iPSCs demonstrated a normal karyotype (Figure 1Cv), maintained identity to the parental LCLs (data not shown), and displayed an IgGH rearrangement profile similar to the parental LCLs (Figure 1Civ). IgGH profiles can serve as a clone tracking tool for LCL-iPSCs and their derivatives.14,15 RT-PCR confirmed expression of pluripotency-associated transcripts (Figure 1Cii; supplemental Figure 1) and the absence of reprogramming elements (Figure 1D-E; supplemental Figure 2). All 4 LCL-iPSCs maintained in the presence of TeSR-2 for more than 25 passages generated well-differentiated teratomas, revealing the presence of cartilage (mesoderm), goblet cells (endoderm), and neural rosettes (ectoderm) (Figure 2D). In vitro differentiation of LCL-iPSCs was performed to assess their endodermal, ectodermal, and mesodermal potential. Generation of α1-antitrypsin-positive hepatocyte-like cells (Figure 2Ei) confirmed endodermal potential. Generation of β3-tubulin-positive neural cultures and β3-tubulin/Nestin double-positive neural precursor cells (Figure 2Eiii-iv) confirmed ectodermal potential. Mesodermal potential was confirmed by generating cardiomyocytes and multipotent HPCs. Fourteen days of cardiac differentiation resulted in 2% to 15% troponin T expression (Figure 2Eii). HPCs were quantified by the presence of CD34+, CD45+, CD43+, CD41+, and CD235a+ expressing cells and methylcellulose-based colony forming assays (Figure 2Ev-vii). LCL-iPSCs derived HPCs were further differentiated to generate macrophages, granulocytes, megakaryocytes, and monocytes.
Analysis of LCL-iPSCs for reprogramming and viral elements and trilineage differentiation of LCL-iPSCs. (A) RT-PCR analysis of H1 (hESC line), LCL-1, LCL-2, and 2 representative LCL-iPSC clones from each donor line at passage 25 for expression of EBV genes: EBNA-1, EBNA-2, LMP-2A, and BZLF-1. GAPDH was used as a positive loading control for each sample, and cDNA made in the absence of reverse transcriptase (no RT) was used to verify that genomic DNA did not contaminate the RNA samples. (B) Immunohistochemistry was performed on LCL-1, LCL-2, and 2 representative LCL-iPS clones from each donor line using an anti–EBNA-1 antibody to detect EBNA-1 protein expression (brown). Images were captured using original magnification ×100. (C) EBV loss during reprogramming is confirmed by quantitative PCR. The viral load during reprogramming was evaluated by harvesting genomic DNA harvested at various passages during the reprogramming. Quantitative PCR was performed using primers, and TaqMan probes targeted 3 EBV gene segments: BamH1W, EBNA-1, and EBER1. The human APOB gene was used for normalization, and the loss of EBNA-1 (i), EBER1 (ii), or BamH1W (iii) was fitted to a general exponential function y = b*fn, where y refers to the copies of viral elements (EBNA-1, EBER1, or BamH1W) per cell for passage n, f is the fraction of daughter cells that contain the virus per passage, and both b and f were chosen to fit the data. (D) H&E staining of teratomas derived from immunodeficient mice injected with LCL-iPS2a shows tissues representing all 3 embryonic germ layers: endoderm (goblet cells, left panel), ectoderm (neural rosettes, middle panel), and mesoderm (cartilage, right panel). All H&E images were captured using original magnification ×40. (E) Trilineage in vitro differentiation. (i) Quantification of α1-antitrypsin-expressing hepatocyte precursors derived from LCL-iPSCs at day 33 by flow cytometry. (ii) Quantification of cardiac troponin T (cTNT)-positive cardiomyocytes derived from LCL-iPSCs at day 14 by flow cytometry. (iii) Neural cultures from LCL-iPS2b immunostained for the presence of β3-tubulin (original magnification × 20). (iv) Quantification of β3-tubulin and nestin-coexpressing neural precursors from neural induced LCL-iPSCs by flow cytometry. (v) Megacult cultures of HPCs derived from LCL-iPS2a cells stained for the presence of megakaryocytes and proplatelets (original magnification ×40; left panel). HPC-derived LCL-iPS2b expanded in the presence of granulocyte-macrophage colony-stimulating factor and stained for the presence of monocytes, neutrophils, and macrophages (original magnification ×20; right panel). (vi) Quantification of colony-forming units (CFU) to demonstrate the presence of erythroid (CFU-E/BFU-E), myeloid composing macrophage (CFU-M), granulocyte (CFU-G), and granulocyte-macrophage (CFU-GM), and multipotent composing granulocyte-erythroid-macrophage-megakaryocyte (CFU-GEMM) colonies from all 4 LCL-iPSCs. (vii) In vitro differentiation into LCL-iPSCs to cells to HPCs via a defined serum-free embryoid body differentiation protocol for 12 days. The percentage of single-positive CD34, CD45, CD43, CD41, and CD235a and double-positive CD34/CD43, CD45/CD43, and CD34/45 cells was quantified by flow cytometry. All images were captured on a Olympus 1×71 microscope equipped with a Olympus DP70 camera and DP Controller Version 3 software
Analysis of LCL-iPSCs for reprogramming and viral elements and trilineage differentiation of LCL-iPSCs. (A) RT-PCR analysis of H1 (hESC line), LCL-1, LCL-2, and 2 representative LCL-iPSC clones from each donor line at passage 25 for expression of EBV genes: EBNA-1, EBNA-2, LMP-2A, and BZLF-1. GAPDH was used as a positive loading control for each sample, and cDNA made in the absence of reverse transcriptase (no RT) was used to verify that genomic DNA did not contaminate the RNA samples. (B) Immunohistochemistry was performed on LCL-1, LCL-2, and 2 representative LCL-iPS clones from each donor line using an anti–EBNA-1 antibody to detect EBNA-1 protein expression (brown). Images were captured using original magnification ×100. (C) EBV loss during reprogramming is confirmed by quantitative PCR. The viral load during reprogramming was evaluated by harvesting genomic DNA harvested at various passages during the reprogramming. Quantitative PCR was performed using primers, and TaqMan probes targeted 3 EBV gene segments: BamH1W, EBNA-1, and EBER1. The human APOB gene was used for normalization, and the loss of EBNA-1 (i), EBER1 (ii), or BamH1W (iii) was fitted to a general exponential function y = b*fn, where y refers to the copies of viral elements (EBNA-1, EBER1, or BamH1W) per cell for passage n, f is the fraction of daughter cells that contain the virus per passage, and both b and f were chosen to fit the data. (D) H&E staining of teratomas derived from immunodeficient mice injected with LCL-iPS2a shows tissues representing all 3 embryonic germ layers: endoderm (goblet cells, left panel), ectoderm (neural rosettes, middle panel), and mesoderm (cartilage, right panel). All H&E images were captured using original magnification ×40. (E) Trilineage in vitro differentiation. (i) Quantification of α1-antitrypsin-expressing hepatocyte precursors derived from LCL-iPSCs at day 33 by flow cytometry. (ii) Quantification of cardiac troponin T (cTNT)-positive cardiomyocytes derived from LCL-iPSCs at day 14 by flow cytometry. (iii) Neural cultures from LCL-iPS2b immunostained for the presence of β3-tubulin (original magnification × 20). (iv) Quantification of β3-tubulin and nestin-coexpressing neural precursors from neural induced LCL-iPSCs by flow cytometry. (v) Megacult cultures of HPCs derived from LCL-iPS2a cells stained for the presence of megakaryocytes and proplatelets (original magnification ×40; left panel). HPC-derived LCL-iPS2b expanded in the presence of granulocyte-macrophage colony-stimulating factor and stained for the presence of monocytes, neutrophils, and macrophages (original magnification ×20; right panel). (vi) Quantification of colony-forming units (CFU) to demonstrate the presence of erythroid (CFU-E/BFU-E), myeloid composing macrophage (CFU-M), granulocyte (CFU-G), and granulocyte-macrophage (CFU-GM), and multipotent composing granulocyte-erythroid-macrophage-megakaryocyte (CFU-GEMM) colonies from all 4 LCL-iPSCs. (vii) In vitro differentiation into LCL-iPSCs to cells to HPCs via a defined serum-free embryoid body differentiation protocol for 12 days. The percentage of single-positive CD34, CD45, CD43, CD41, and CD235a and double-positive CD34/CD43, CD45/CD43, and CD34/45 cells was quantified by flow cytometry. All images were captured on a Olympus 1×71 microscope equipped with a Olympus DP70 camera and DP Controller Version 3 software
Because EBNA-1 is required for the establishment of latent EBV infection and long-term survival of LCLs,16,17 and is the only viral protein required for persistence of EBV in host cells, LCL-iPSCs were tested for the presence of EBNA-1. EBNA-1 was not detectable at the transcriptional and protein levels in the LCL-iPSCs after 25 passages (Figure 2A-B). In addition, no expression of other viral genes (EBNA-2, LMP-2A, and BZLF-1; Figure 2A) or the viral sequences associated with these genes (supplemental Figure 2) was detectable, further supporting the loss of EBV from LCL-iPSCs.
Earlier reports18,19 have described the unequal partitioning of EBV in the absence of viral selection in daughter cells. To detect the rate of loss of EBV-associated viral elements in LCL-iPSCs, real-time quantitative PCR was performed to measure viral load in parental LCLs and LCL-iPSCs. The quantification of 3 EBV genome segments (EBNA-1, EBER1, and BamH1W) was performed along with a control human gene (APOB) by which to normalize between samples.20 The absolute copy number of the EBV-associated viral elements present at various passage numbers was curve fitted to a general exponential function y = b*fn, where y refers to the copies of viral elements (EBNA-1, EBER1, or BamH1W) per cell for passage n (of LCL-iPSCs), f is the fraction of daughter cells that contain the virus per passage, and both b and f were chosen to fit the data. The results demonstrated that only 46% EBNA-1 (Figure 2Ci), 10% EBER1 (Figure 2Cii), and 40% BamH1W (Figure 2Ciii) were retained per passage of LCL-1-iPSCs. Similarly, 18% of EBNA-1, 0.52% EBER1, and 0.87% BamH1W were retained per passage of LCL-2-iPSCs (data not shown). The results demonstrated an exponential decay and the complete loss EBV as early as the third passage of an LCL-2-iPSC and 10th passage of an LCL-1-iPSC.
In conclusion, episomal reprogramming of LCLs leads to accelerated loss of EBV to generate EBV-free LCL-iPSCs, which can be used to generate defined cell lineages. LCL-iPSCs can serve as a valuable tool to further researching a myriad of immunologic, epidemiologic, and rare disease studies.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Rachel Lewis, Cellular Dynamics International, for teratoma injections of iPSCs; Sarah Burton, Cellular Dynamics International, for assistance with hematopoietic differentiation of iPSCs; Monica Strathman, Casey Stankewicz, and Nate Meyer, Cellular Dynamics International, for assistance with neural differentiation of iPSCs; Melissa Iburg and Jennifer Luebke-Wheeler, Cellular Dynamics International, for assistance with endodermal differentiation of iPSCs; Ruth Sullivan and Annette Gendron-Fitzpatrick, Comparative Pathology and Laboratory Services RARC, for pathologic review of teratoma samples; Drew Ronneburg, Department of Surgery, Histological Core Services University of Wisconsin-Madison, for immunohistochemical staining of teratoma slides; Margaret Gulley, University of North Carolina-Chapel Hill, for assistance with the quantification of viral load in parental LCLs as well as LCL-iPSCs; Emile Nuwaysir, Michael Miller, Amanda Mack, Giorgia Salvagiotto, and Tom Burke, Cellular Dynamics International, for helpful scientific discussion and critical review of the manuscript; and Igor Slukvin and Shannon Kenney, University of Wisconsin-Madison, for helpful scientific discussion and critical review of the manuscript.
Authorship
Contribution: D.R. designed and conducted experiments, performed research, analyzed data, made figures, and wrote this paper; S.J.D. designed and conducted experiments, performed research, analyzed data, made figures, and assisted in writing this paper; J.Y. derived the method and media formulation for feeder-free episomal reprogramming and contributed reagents and materials; M.E.B. designed and conducted experiments and analyzed data; J.A.T. conceived of the idea and provided scientific advice; and N.J.S. supervised the research project.
Conflict-of-interest disclosure: J.A.T. is a founder, stock owner, consultant, and board member of Cellular Dynamics International, and serves as a scientific advisor to and has financial interests in Tactics II stem cell venture. All authors are employed by, and have a financial interest in, Cellular Dynamics International Inc. In addition, some of the authors are listed as inventors on a patent application related to the works presented in this paper. This does not alter the authors' adherence to all Blood policies on sharing data and materials.
Correspondence: Deepika Rajesh, Cellular Dynamics International Inc, 525 Science Dr, Suite 200, Madison, WI 53711-1018; e-mail: drajesh@cellulardynamics.com.