Abstract
The Hedgehog pathway is a critical mediator of embryonic patterning and organ development, including hematopoiesis. It influences stem cell fate, differentiation, proliferation, and apoptosis in responsive tissues. In adult organisms, hedgehog pathway activity is required for aspects of tissue maintenance and regeneration; however, there is increasing awareness that abnormal hedgehog signaling is associated with malignancy. Hedgehog signaling is critical for early hematopoietic development, but there is controversy over its role in normal hematopoiesis in adult organisms where it may be dispensable. Conversely, hedgehog signaling appears to be an important survival and proliferation signal for a spectrum of hematologic malignancies. Furthermore, hedgehog signaling may be critical for the maintenance and expansion of leukemic stem cells and therefore provides a possible mechanism to selectively target these primitive cell subpopulations, which are resistant to conventional chemotherapy. Indeed, phase 1 clinical trials of hedgehog pathway inhibitors are currently underway to test this hypothesis in myeloid leukemias. This review covers: (1) the hedgehog pathway and its role in normal and malignant hematopoiesis, (2) the recent development of clinical grade small molecule inhibitors of the pathway, and (3) the potential utility of hedgehog pathway inhibition as a therapeutic strategy in hemato-oncology.
Introduction
The hedgehog (Hh) signaling pathway was initially discovered by Nüsslein-Volhard and Weischaus in 1980 through a genetic screen for factors influencing Drosophila embryonic patterning.1 Characterization of the hh gene revealed that it encodes a secreted protein expressed in a repeated pattern across the Drosophila embryo. Absence of this HH protein prevented normal segmentation and gave the Drosophila embryo a characteristic “prickly” appearance reminiscent of a curled hedgehog. As studies progressed, it became clear that Hh signaling is a conserved process between species and is critically important in vertebrate embryogenesis where it is required for development of internal organ, midline, and neurologic structures, limb patterning, and development of the hematopoietic system. It has been well established that absence of functional Hh signaling causes dysmorphisms, such as holoprosencephaly (cyclopia), limb abnormalities, and improper biologic system and organ development.2,3
Hh signaling exerts its biologic effect through controlling the behavior of stem cells within the target tissue. Hh concentration gradients are generated and, in concert with or in opposition to other similar signaling pathways, exert a topologic and time-dependent influence on the apoptosis, proliferation, and differentiation programs of local stem and progenitor cells. Thus, populations of tissue-specific stem and progenitor cells can be driven to expand or contract and guided toward a particular specialized function.3-6
After its critical role in embryogenesis, Hh signaling remains active in a more limited extent throughout the life of the organism where it plays a key role in the maintenance and expansion of somatic stem cell populations through modulation of self-renewal activity. It is important in response to injury, tissue stress, healing, and regeneration.7-10
Interest in this pathway has been maintained and strengthened by the recent realization that inappropriate activation of Hh signaling is associated with many disparate human malignancies (including some hematologic malignancies).8,10-14 Furthermore, recent evidence suggests that Hh signaling is critical for the maintenance and expansion of malignant stem cells, placing Hh signaling at the very heart of the cancer stem cell (CSC) hypothesis and a key candidate for stem cell-directed anti-leukemia or anti-tumor therapy.13,15-18
In this review, we focus on the nature of the Hh signaling pathway and its relevance to normal and malignant hematopoiesis, with a particular focus on the recent developments in the laboratory and in early clinical trials, suggesting that Hh signaling blockade alone or in combination with other treatments is a new and potentially effective intervention in hematologic malignancies.
The Hh signaling pathway
Hh is a ligand-dependent signaling pathway. Secretory cells produce 3 possible isoforms of the HH ligand: Sonic (SHH), Desert (DHH), or Indian (IHH) Hh. These are initially 45-kDa precursor proteins, which are cleaved and subjected to cholesterol and palmitoyl modification to produce an active N-terminal fragment of 19 kDa.19,20 These proteins are similar in structure and may be partially redundant in function; however, they also have tissue-specific roles in the developing organism and in the adult stem cell microenvironment.21 SHH influences the development of many tissues in the embryo, IHH is produced in hematopoietic tissue and bone and has a role in early hematologic development, and DHH is expressed in the testes and nervous system where deficiency leads to male sterility and peripheral nerve defects.2,6,22
Hh signaling requires strict spatial limitation and tight modulation. Numerous proteins are involved in receiving and transmitting the Hh signal to the nucleus; positive feedback loops accentuate and maintain the signal and negative feedback loops switch off the pathway after signal activation.
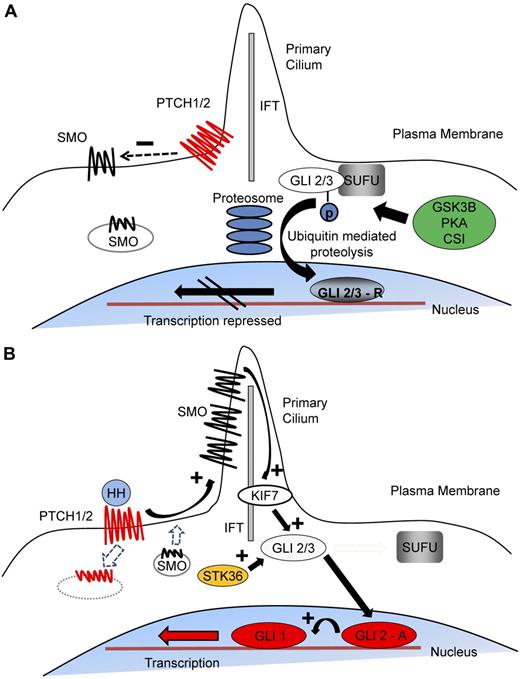
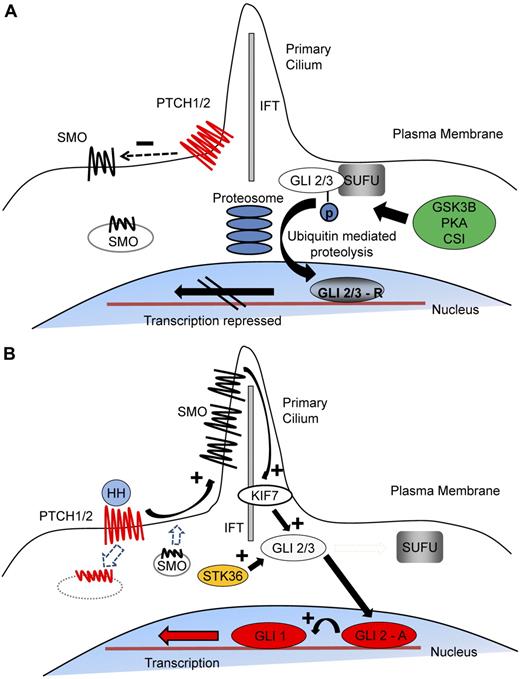
The central components of the pathway are composed of a pair of 12-span transmembrane receptor proteins, patched (PTCH) 1 and 2; a 7-span transmembrane protein, smoothened (SMO); and the family of Glioma (GLI) zinc finger transcription factors GLI1, GLI2, and GLI3 (Figure 1). Unusually, the Hh receptor PTCH is a negative regulator of pathway activity, whereas the immediately downstream element SMO is the major positive regulator. In the resting state, PTCH represses SMO activity, but after Hh binding this repression is removed.23 The mechanism of signal transduction between PTCH and SMO in vertebrates is not known, but the 2 receptors do not appear to interact directly. Patched proteins bear a striking homology to a transmembrane lipid transporter protein (Neimann-Pick C1 protein), and SMO appears to belong to the G-protein coupled receptor family.24,25 Current evidence suggests that PTCH influences SMO activity through oxysterol trafficking. Oxysterols activate Hh signaling through SMO, whereas secretion of pro-vitamin D3 is inhibitory.26,27 After receptor ligand interaction, PTCH is internalized, SMO accumulates on the plasma membrane and interacts with the GLI family of transcription factors.28 Whereas GLI3 is predominantly a transcriptional repressor, GLI2 exists in both a full-length active form and a truncated repressor form.29,30 Activated SMO alters the balance between these forms.10,30 In many vertebrate cell types, this signaling occurs within the primary cilium.31,32 SMO and GLI proteins accumulate there through interaction with the intraflagellar transport (IFT) proteins facilitating activation and onward transduction of the Hh signal.30,31,33 However, this is dispensable in hematopoietic cells as they appear not to possess primary cilia, although, interestingly, they do express IFT proteins.34
The mechanism of Hh signal transduction. (A) In the resting state, PTCH 1/2 is expressed on the plasma membrane and acts to repress SMO activity by preventing its expression and localization to the primary cilium. GLI2/3 transcription factors are within a complex, including SUFU, an inhibitor of Hh signaling. This conformation promotes nonspecific phosphorylation of the C terminus by GSK3β, CSI, and PKA, resulting in E3 ubiquitin ligase activity and subsequent partial proteosomal proteolysis to the C terminal truncated repressor form. After translocation to the nucleus, the repressive forms of GLI2 (GLI2-R) and particularly GLI3 (GLI-3R) potently inhibit the Hh transcriptional program. (B) Interaction of HH ligand with PTCH promotes PTCH internalization and degradation and releases the repression of SMO, causing its accumulation within the primary cilium. Active SMO in the primary cilium stabilizes the full-length forms of GLI2 (GLI2-A) and GLI3 (GLI3-A) and accentuates the effect of other positive regulators of Hh signaling, including serine threonine kinase 36 (STK36) and kinesin family member 7 (KIF7), which may be involved in translocation of GLI into the primary cilium. After translocation to the nucleus, GLI2-A potently activates transcription of downstream Hh targets, including GLI1 and PTCH1, and influences chromatin conformation, apoptosis, cell cycle activity, and differentiation.
The mechanism of Hh signal transduction. (A) In the resting state, PTCH 1/2 is expressed on the plasma membrane and acts to repress SMO activity by preventing its expression and localization to the primary cilium. GLI2/3 transcription factors are within a complex, including SUFU, an inhibitor of Hh signaling. This conformation promotes nonspecific phosphorylation of the C terminus by GSK3β, CSI, and PKA, resulting in E3 ubiquitin ligase activity and subsequent partial proteosomal proteolysis to the C terminal truncated repressor form. After translocation to the nucleus, the repressive forms of GLI2 (GLI2-R) and particularly GLI3 (GLI-3R) potently inhibit the Hh transcriptional program. (B) Interaction of HH ligand with PTCH promotes PTCH internalization and degradation and releases the repression of SMO, causing its accumulation within the primary cilium. Active SMO in the primary cilium stabilizes the full-length forms of GLI2 (GLI2-A) and GLI3 (GLI3-A) and accentuates the effect of other positive regulators of Hh signaling, including serine threonine kinase 36 (STK36) and kinesin family member 7 (KIF7), which may be involved in translocation of GLI into the primary cilium. After translocation to the nucleus, GLI2-A potently activates transcription of downstream Hh targets, including GLI1 and PTCH1, and influences chromatin conformation, apoptosis, cell cycle activity, and differentiation.
When Hh signaling is “off,” GLI2 and GLI3 are retained in the cytoplasm by a protein complex, including the inhibitory molecule suppressor of fused (SUFU) and are phosphorylated by nonspecific kinase activity mediated by glycogen synthase kinase 3β (GSK3 β), casein kinase (CSI), and protein kinase A (PKA).35-38 After phosphorylation, GLI2 and GLI3 undergo C-terminal ubiquitination and partial proteosome-mediated proteolysis to the truncated inhibitory form before nuclear translocation, resulting in repression of the pathway.37 In the presence of Hh ligand, GLI2 and GLI3 phosphorylation is prevented and full-length active forms of the transcription factors translocate to the nucleus.29,38 This activates the transcription of downstream targets that include both positive (GLI1) and negative (PTCH1/2) regulatory elements, which drive the Hh transcription program and down-regulate ongoing signaling, respectively.30
Hh signaling and hematopoiesis
Hh signaling has multiple complex roles in both adult and embryonic hematopoiesis, depending on the stage of development and whether the hematopoietic system is under regenerative pressure. IHH, expressed by endodermal cells, specifies hematopoietic differentiation at the earliest stages of primitive hematopoiesis and has roles in hematopoietic and vascular development.5,6 However 50% of Ihh null mice survive, suggesting that IHH functions are partially redundant.39 Definitive hematopoiesis is the second wave of hematopoietic activity characterized by the development of hematopoietic stem cells (HSCs). This process is initiated in the aorta-gonad-mesonephros region but relocates to the fetal liver and subsequently the bone marrow.40 Studies in zebrafish and mice indicate that Hh signaling has a role in establishing definitive hematopoiesis.5,41,42 Furthermore, HH ligand has been shown to expand definitive hematopoietic progenitors in mice and humans.5,43,44
Early studies of adult hematopoiesis suggested that Hh signaling caused expansion and increased functional activity of the HSC compartment.9,43 More recently, there has been controversy over the role, if any, that Hh signaling plays in adult hematopoiesis because of the differing results of murine studies dissecting the role of Hh mediators in adult hematopoiesis.
Dierks et al13 and Trowbridge et al9 demonstrated that Ptch1 heterozygosity (hence Hh activation) was associated with increased stem cell number, faster hematologic recovery after challenge with 5-fluorouracil, and increased transplantability in murine models. In addition, Trowbridge et al found that long-term repopulating cells (the most primitive HSCs) were ultimately exhausted through constant Hh activation.9 In contrast to this, Dierks et al found no diminution of long-term HSC function.13 Siggins et al examined adult mice subject to conditional deletion of Ptch1 in various tissues, including primitive hematopoietic cells demonstrating that conditional deletion of Ptch1 increased circulating primitive hematopoietic cells but did not result in enhanced engraftment in transplantation experiments or exhaustion of long-term repopulating capacity.45 Furthermore, their experiments suggested that Ptch1 deletion only altered proliferation and mobilization of HSCs when occurring within the supporting bone marrow stroma as, when specific deletion limited to HSCs was performed, these differences disappeared. This suggests that the effects are through signaling extrinsic to the HSCs and not a direct effect of Hh on the HSCs themselves.45
These discrepancies may be partly explained by the alternative experimental approaches used. Dierks et al used fetal liver HSCs from Ptch1+/− embryos,13 whereas Trowbridge et al studied adult Ptch1+/− HSCs.9 In these studies, Ptch1 deletion was present during embryogenesis. In the germline mutant, Ptch1 heterozygosity would be a feature of all cells and tissues rather than being confined to the hematopoietic system. In contrast, Siggins et al used conditional and targeted approaches using the Mx-Cre system.45 They induced deletion of Ptch1 in hematopoietic tissue of mature mice and also used the SCL enhancer to target Ptch1 deletion to adult murine HSCs.45
Because absence of SMO is lethal, analysis of Smo null mutants is not possible. Four groups have investigated the effect of Smo deletion, either through recovery of Smo null HSCs from fetal liver or through 2 different conditional deletion methodologies.13,17,46,47 Dierks et al found no significant difference in the behavior of fetal HSCs recovered from Smo null mice compared with normal mice.13 Gao et al46 and Hoffman et al47 used the Mx1-Cre system to create a murine model where Smo deletion could be induced. Neither found any significant difference in the short- or long-term measures of hematopoiesis after deletion of Smo and therefore abrogation of Hh signaling. In contrast, Zhao et al demonstrated profound reduction in stem cell activity as indicated by secondary transplant capacity after Vav-driven Cre-Lox–mediated conditional Smo deletion.17
Although on the surface these conflicts appear irreconcilable, the alternative experimental strategies go some way to explaining these differences; the Mx1-Cre system allows deletion in adulthood and predominantly affects hematopoietic and liver cells, whereas the Vav-Cre-Lox system is active throughout embryogenesis and is less selective, affecting both hematopoietic and endothelial tissue, raising the possibility that Hh signaling was disrupted in a wider range of tissues and at an earlier time point.13,17,46,47
Genetic studies have also been performed on the main downstream mediators of Hh signaling. Merchant et al characterized the effect of Gli1 deletion on hematopoiesis in a Gli1 null murine model.48 No abnormalities in gross hematopoiesis were found; however, there was a reduction in proliferation within the stem and myeloid progenitor compartments as well as a reduction in myeloid differentiation and delayed recovery after 5-fluorouracil exposure.
Hh acts in concert with other morphogenic signals to influence development of T and B lymphocytes. Thymic stroma and T cells both express Hh pathway mediators.49,50 Early studies suggested that Hh signaling negatively regulated T-cell development51 ; however, subsequent work indicates that Hh signaling has a positive regulatory role in early T-cell development.45,49,50,52-54 Both IHH and SHH affect T-cell proliferation and maturation.49,52 Conditional deletion of Smo at different levels of T-cell development, performed by El Andaloussi et al, suggested that abrogation of Smo expression mainly affects primitive thymocytes, leading to thymic atrophy and profound defects in early T-cell survival, proliferation, and maturation.50 Uhmann et al studied a Ptch1 conditional deletion murine model and demonstrated that knockout of Ptch1 led to profound loss of mature T and B cells.53,54 Siggins et al demonstrated that Ptch1 deletion led to significant apoptosis in pre-B cells, blocked T-cell specification in bone marrow T cells, and caused apoptosis of CD4+CD8+ T cells because of deletion of Ptch1 in the supporting microenvironment.45,54
Overall, it appears that Hh signaling has effects on the hematopoietic system dependent on developmental stage and cell lineage. These effects are the result of a complex interplay between the cells and their microenvironment at certain developmental stages rather than being purely hematopoietic cell-intrinsic mechanisms. It is interesting to note that, in early clinical trials of SMO inhibition in humans, no hematologic toxicities have been noted with up to 6 months of exposure.55 Thus, although Hh signaling may have a role in normal adult hematopoiesis, it is probably dispensable, at least in steady-state conditions, providing a therapeutic window that may be exploited in hematologic and other malignancies.
Hh and malignancy
Abnormal Hh signaling is associated with diverse human malignancies.56 Its oncogenic properties were first identified through the realization that the genetic abnormality causing Gorlin syndrome (associated with an excess risk of rhabdomyosarcoma, medulloblastoma, and basal cell carcinoma) is an inherited inactivating PTCH mutation.57 Sporadic cases of the same malignancies are frequently associated with either inactivating mutations of PTCH or activating mutations of SMO, indicating that PTCH and SMO act as tumor suppressor and oncogene, respectively.56 Further work confirmed that GLI transcription factors were responsible for driving tumor formation.58 The association of Hh signaling with oncogenesis is not surprising given the critical role that Hh signaling performs in regulating cell proliferation, cell cycle machinery, apoptosis, chromatin modeling, self-renewal, and epithelial-to-mesenchymal transition in responsive cells.59
Recent evidence suggests that Hh signaling may have distinct mechanisms of action in different tumor environments. For example, in basal cell carcinoma and medulloblastoma, the most common lesions in Hh signaling are gain-of-function SMO mutations or loss-of-function PTCH mutations.11,60 These are rare in glioblastoma and lymphoma; however, Hh signaling remains critically important as, in these tumors, malignant cells respond to HH ligand secreted from the surrounding microenvironment.12,61 Furthermore, although Hh signaling is important in pancreatic cancer tumorigenesis, this is not through direct signaling to tumor cells but rather because of HH ligand production by tumor cells interacting with the local stroma.62 Thus, Hh signaling appears to be associated with development and maintenance of malignancy through (1) ligand-independent signaling resulting from cell-intrinsic mutations or (2) autocrine/paracrine signaling between tumor cells and stroma or vice versa. Lastly, there is accumulating evidence that CSCs are dependent on Hh signaling for population maintenance and expansion.
Malignant stem cells
The CSC hypothesis suggests that tumors are hierarchical structures where the capacity for tumor initiation and propagation is limited to a small number of very primitive cells within the tumor bulk. These cells exhibit similar characteristics to normal stem cells, including the ability to undergo symmetric and asymmetric self-renewal divisions, thereby maintaining or expanding their number in addition to giving rise to more differentiated progeny.63 The existence of such a population has been conclusively demonstrated in chronic myeloid leukemia (CML) and acute myeloid leukemia (AML), and there is accumulating evidence for their existence in other hematologic and solid tumors, such as myeloma, lymphoma, glioblastoma, breast, and prostate cancer.16,18,64-67 In these malignancies, CSCs are predominantly quiescent and therefore resistant to conventional therapeutic approaches. Failure to effectively target these cells results in residual low-level disease and the likelihood of future relapse. If CSCs are dependent on Hh signaling as emerging data suggest, inhibitors of Hh signaling may be excellent CSC-targeting therapies.
Targeting the Hh pathway
As SMO is the main positive regulator, it has become a logical pharmaceutical target in modulating ligand-dependent Hh signaling. The first Hh inhibitor cyclopamine was identified more than 50 years ago after investigation into a spate of birth defects, including cyclopia, in lambs born in sheep farms across Idaho. It transpired that pregnant ewes were grazing on the corn lily Veratrum californicum, a rich source of steroidal alkaloids, including cyclopamine. Cyclopamine was subsequently found to be a potent inhibitor of SMO with anti–tumor activity in in vitro and in vivo systems.68 Although cyclopamine is an effective inhibitor of Hh signaling, it is relatively nonspecific and has significant toxicities and therefore has not been effectively used clinically. However, these results provided impetus to synthesize and test derivatives of cyclopamine or to screen large-scale synthetic molecule libraries for agents with anti-SMO activity. Several years on, there are now several clinical grade SMO inhibitors undergoing preclinical evaluation or early-stage clinical trials (Table 1).
An orally active agent, GDC-0449, showed significant (> 50% response) clinical efficacy against Hh-driven malignancies, such as advanced or metastatic basal cell carcinoma in a phase 1 clinical trial.55 A subsequent study reported that other solid malignancies did not respond, although the participants had advanced, multiply treated malignancies with relatively short follow-up limiting the likelihood of a positive result.69 In both cases, SMO inhibition was well tolerated with little toxicity (predominantly low-grade fatigue, hyponatremia, and dysgeusia); no maximum tolerated dose was reached. Notably, there was a lack of hematologic toxicity in treated patients.55,69
Hematologic malignancy
There is great interest in using anti-Hh therapies in hematologic malignancies. This extends from accumulating evidence suggesting that Hh signaling may be critical in the genesis, maintenance, progression, and relapse of various hematologic conditions through both direct and indirect mechanisms. Attention has particularly focused on CML and myeloma where Hh signaling has been implicated in CSC persistence despite conventional therapy.
CML
CML is probably the best understood hematologic malignancy. We know a great deal about its clinical behavior and pathophysiology at the cellular and molecular level. It is a paradigm of a stem cell-driven cancer and is an excellent model for studying stem cell-directed therapies. CML is a clonal disorder driven by the constitutively active oncogenic tyrosine kinase BCR-ABL. The development of tyrosine kinase inhibitors (TKIs) that block BCR-ABL kinase activity, such as imatinib, nilotinib (Glivec & Tasigna; Novartis Pharma), and dasatinib (Sprycel; Bristol-Myers Squibb), radically improved management of CML, leading to unprecedented levels of cytogenetic and molecular responses in chronic-phase patients.70 However, TKI resistance and disease persistence despite TKI therapy remain ongoing issues. Even complete molecular response is not synonymous with cure as increasingly sensitive molecular analysis reveals evidence of persistent disease, with the majority of patients having molecular recurrence after TKI withdrawal.71,72 One reason for disease persistence despite prolonged TKI therapy is that, while harboring the BCR-ABL fusion protein, primitive CML cells are resistant to pharmacologically achievable concentrations of TKI and may not be dependent on BCR-ABL signaling for survival.70,73
Hematopoiesis in chronic-phase CML remains hierarchical with a leukemic stem cell (LSC) giving rise to leukemic progenitor and effector cells. As CML progresses, the hierarchy is disrupted and mature committed progenitors appear to aberrantly reacquire self-renewal capacity through cooperating events (eg, activation of Wnt signaling).74 Therefore, in CML, self-renewal is a potential target both in chronic- and advanced-phase disease.
Hh signaling is increased in BCR-ABL+ stem and progenitor cells, becoming more active with disease progression.13,17,75 Two groups have explored the effect of Smo deletion in murine models of CML. Zhao et al used the Vav-Cre-Lox system to create Smo-deficient mice from which to isolate Smo−/− HSCs,17 whereas Dierks et al used fetal liver cells from Smo-deficient mouse embryos.13 Both groups expressed Bcr-Abl in these cells before transplantation. Despite differing approaches, broadly similar results were obtained. Smo deletion reduced LSC numbers and reduced incidence of leukemia with prolonged latency in primary transplantation and greatly reduced capacity to recrudesce disease in secondary hosts. Both groups performed complementary pharmacologic inhibitor studies, demonstrating prolonged survival in diseased mice, reduced LSC population, and lower functional activity in vivo and in vitro after cyclopamine treatment.13,17 Interestingly, the combination of TKI therapy with cyclopamine resulted in the largest reduction in LSCs in vitro and in vivo.13
Studies using clinical grade SMO inhibitors alone and combined with TKIs both in vitro and in vivo support these conclusions demonstrating significant reduction in measures of self-renewal, incidence of leukemia in secondary transplant recipients, and extended survival.76,77 Therefore, Hh signaling is active in CML, is critical to the maintenance and expansion of the diseased stem/progenitor cells, and presents an exciting new target in CML. Phase 1 trials testing the safety of combining TKI and Hh inhibition in patients with CML of all stages are now open (Table 1; NCT00953758, NCT01218477, NCT1456676).
Multiple myeloma
Myeloma is a malignancy characterized by the malignant clonal expansion of plasma cells and is associated with the production of monoclonal immunoglobulin. A variety of therapeutic approaches have been used but, unfortunately for the majority, myeloma remains incurable because of multiple relapse and progression. Evidence is accumulating that myeloma is maintained from a small population of myeloma stem cells, which are resistant to current therapies and may be responsible for the relapsing natural history of the disease.78 Matsui et al demonstrated that a small population of postgerminal center memory B cells with the surface phenotype CD138−/CD19+/CD27+ exist within the tumor, are clonally related to the circulating tumor bulk, and appear to exhibit stem cell-like characteristics.79,80 These cells are capable of in vitro colony formation, serial replating, and transplanting the original myeloma clone into secondary hosts.79,80 In addition, they express constituents of the Hh pathway; and whereas exogenous HH ligand caused expansion, inhibition with cyclopamine or a SMO blocking antibody resulted in contraction of the putative CSC compartment.18 Dierks et al demonstrated that HH ligand from supporting stroma was required for in vitro survival and expansion of murine and human primary lymphoma and myeloma cells.12 These observations are particularly relevant as primitive myeloma cells appear to be resistant to standard myeloma therapies, including lenalidomide, bortezomib, dexamethasone, and cyclophosphamide.80
Acute leukemia
Less is known about the Hh signaling pathway and its influence on AML and acute lymphoid leukemia (ALL). Although there is clear evidence for a LSC population in AML and ALL, recent work has suggested that this population is phenotypically variable between patients, may not be confined to a single clonal subpopulation, and may arise from an HSC or a committed progenitor.81,82 Cells with LSC properties have reduced sensitivity to chemotherapeutic agents and contribute to treatment failure and disease relapse.83 Therefore, there is a clear rationale for investigating and targeting mechanisms involved in LSC maintenance and self-renewal. A variety of cell-extrinsic mechanisms are involved in this process, including oxidative stress, cell-cell contact, and microenvironmental signaling in addition to cell intrinsic mechanisms, such as constitutive activation of NFκB/AKT/PI3K, overexpression of anti-apoptosis mechanisms, and chromatin modification. Furthermore, the leukemogenic translocation is sometimes capable of enhancing or conferring self-renewal activity. For example, AML1-ETO translocations interact with the downstream amino-terminal enhancer of split (AES), enhancing self-renewal measurements in vitro, and the MOZ-TIF2 and MLL-ENL translocations confer self-renewal properties to progenitor cells.84,85 In this context, blocking one pathway, such as Hh, may not be sufficient to target these LSCs. Hh signaling is completely dispensable for the development of acute leukemia in a MLL-AF9-mediated murine model of myeloid leukemia and a Notch-dependent murine model of T-ALL.46,86 In contrast, very recent work in a murine model of erythroleukemia suggested that development of transplantable leukemia depended on proviral activation of Sp1/Pu.1 in cells with an intact Hh signaling pathway.87 In addition, SHH and GLI1 are expressed in leukemic cell lines and primary leukemic blasts, and recent evidence suggests that inhibitors of the Hh pathway may have some efficacy.88-90 Lin et al demonstrated Hh signaling activity in precursor B-ALL and that SMO inhibition with cyclopamine or IPI926 reduced in vitro and in vivo measures of self-renewal.91 Another preliminary study indicated that cyclopamine has some efficacy in AML in vitro, possibly via mitigation of multidrug resistance.92
In CSC-driven hematologic malignancies, the rationale for SMO inhibition is predominantly to target the resistant, diseased stem cell population, attempting to reduce relapse rate and potentially cure these diseases. Although it appears that both CML and myeloma stem cells rely on Hh signaling for maintenance and expansion, it is not clear whether this is a cell-intrinsic property, driven by autocrine/paracrine production of HH ligand, or consequent on the effect of Hh signaling on the supportive stromal microenvironment.
Lymphoma and CLL
Hh pathway inhibition may also be effective in lymphoma and chronic lymphocytic leukemia (CLL). Hh signaling is critical for normal B- and T-cell development; however, it is primarily the microenvironmental cells and supportive stroma of the bone marrow and lymphoid organs that produce the HH ligand, which is required for lymphoid cell maintenance.45,54 Constituents and targets of Hh signaling are expressed in various lymphoma cell lines and primary tissue.92-94 IHH and SHH have been shown to be survival factors in B-cell malignancies.94 Dierks et al used the Eμ-myc murine model of Burkitt lymphoma to demonstrate that stromal coculture was necessary for lymphoma cell survival and expansion, but stroma could be effectively replaced with soluble SHH or IHH.12 Furthermore, lymphoma cells underwent apoptosis in the absence or inhibition of Hh signaling both in vitro and in vivo. Downstream Hh targets included BCL-2 and BCL-XL; both these pro-survival pathways were up-regulated in the presence of Hh signaling and down-regulated after inhibition.12,94
In mantle cell lymphoma, preliminary work has shown that mantle cell lymphoma cell lines and primary human samples had increased expression of Hh pathway components compared with normal B cells and were partially responsive to HH ligand or its pharmacologic inhibition.95 Direct inhibition of the downstream effectors GLI1 and GLI2 had the most profound effect on mantle cell lymphoma cells, indicating that, although canonical Hh signaling may be involved in mantle cell lymphoma, there are probably other factors driving GLI1 and GLI2 expression.
Inhibitors of Hh signaling may also have a role in future treatment of CLL, as initial observations suggest that mediators and downstream targets of Hh signaling (GLI1, GLI2, and SUFU) are up-regulated in B-CLL cells and may correlate with clinical outcome.96 Pharmacologic inhibition of Hh signaling abrogated stromal microenvironment-mediated survival of B-CLL cells in in vitro treatment assays with fludarabine.96 In contrast, Desch et al found that key participants of the Hh signaling cascade (including SMO and GLI1) were not differentially expressed in B-CLL cells over normal B cells.97 In addition, in their studies, SMO inhibition alone did not influence B-CLL cell survival in vitro. However, GANT61 (a direct Gli1 inhibitor) caused significant apoptosis in B-CLL cells but not normal B cells in vitro, which could be rescued by stromal coculture but not recombinant SHH ligand alone. This suggests that other signaling pathways converging on GLI1 expression were responsible.97 Decker et al recently demonstrated that both Hh mediator expression and SMO inhibitor responsiveness were variable in different patients. They found that 60% of their CLL cohort responded to SMO inhibition.98 Factors that predicted likelihood of response included elevated expression of GLI1 and PTCH1 and carriage of trisomy 12. In addition, trisomy 12 CLL cells produced DHH, suggesting that autocrine signaling may be important in this subtype.98
Hh has been implicated in the etiology of T-cell lymphomas. Singh et al demonstrated that constituents of the Hh pathway were overexpressed in ALK+ anaplastic large cell lymphoma.99 They demonstrated amplification of the SHH gene locus and consequently increased levels of mRNA and protein in ALK+ anaplastic large cell lymphoma cell lines and primary tissue and overexpression of GLI1 through PI3K/AKT pathway signaling. They also confirmed that pharmacologic inhibition of SMO led to cell cycle arrest and apoptosis.99 More recently, it has been reported that GLI3 is highly expressed in Hodgkin lymphoma cell lines and in Reed-Sternberg cells from 39 of 39 cases of classic Hodgkin lymphoma by immunohistochemistry, suggesting a hitherto unknown role for Hh signaling in Hodgkin lymphoma.100
Conclusion
In conclusion, despite continued progress in our understanding of the molecular and cellular events that underlie the development and progression of hematologic malignancies, in most instances, complete eradication of the malignant clone remains elusive. This has resulted in long-term dependence on drug therapy to maintain disease control and prevent disease progression and relapse or treatment failure.
It has become increasingly clear that the relationship between the tumor cell and its supporting environment plays a critical role in treatment resistance through direct pro-survival signaling, control of proliferation, and, at least in some malignancies, the maintenance and expansion of CSCs. These relationships are highly complex and are modulated by prevailing chemical conditions, such as oxygen tension, and physiologic cues in addition to a network of signaling pathways, including the conserved embryonic signaling pathway Hh. Targeting these interactions might provide an alternative, more effective therapeutic strategy either alone or in combination with conventional treatments. Hh signaling is an attractive target as there is a large body of evidence that relates abnormal Hh signaling to malignancy; furthermore, from a drug development perspective, inhibition of the key positive regulator SMO is readily achieved. A critical question as to whether SMO inhibition would be therapeutically useful in hematologic malignancies relates to the anticipated level of hematologic toxicity in humans. Clinical grade SMO inhibitors are currently under trial in both solid tumors and hematologic malignancies; interestingly, there appears to be little hematologic toxicity experienced by trial participants.55
The next question relates to the activity and function of Hh signaling in hematopoietic malignancies. Hh signaling intermediates are expressed by cells from a wide spectrum of hemato-oncologic conditions, and Hh signaling appears to exert its effect either through direction of CSC fate or as a survival and proliferation signal derived from the supporting stromal microenvironment as has been shown in models of lymphoma. The degree of evidence that Hh activity is a legitimate target in different hematologic malignancies is variable. There is greatest preclinical evidence to support the use of Hh antagonists in the context of CML where in vitro and in vivo inhibitor studies in mouse and human tissue have demonstrated a significant anti-LSC effect. These results are supported by the complementary genetic studies of Zhao et al17 and Dierks et al13 It must be borne in mind that these were performed using models that resulted in quite different data regarding the requirement for Smo in normal HSCs, where Smo deletion was not specific to HSCs and occurred early in hematopoietic development, conceivably affecting microenvironmental interactions that are subsequently reflected in adult HSC function.
In the context of acute leukemias, the published data are inconsistent and it is probable that the contribution of Hh signaling, and hence the likelihood of benefit from Hh antagonism, is more contextual depending on the transforming mutation. Lastly, in lymphoid malignancies, Hh antagonism could conceivably be used to reduce the pro-survival effect of the tumor microenvironment.
Ultimately, the preclinical data suggest that Hh antagonism may be an extremely useful therapeutic intervention in several hematologic malignancies where it may address the persistence of CSC and the protective effect of the tumor microenvironment; however, it remains to be seen whether or how many of these laboratory observations translate to real clinical benefits to patients.
Acknowledgments
D.A.I. was supported by the Chief Scientist Office, Scotland (clinical research fellowship) and the Greater Glasgow and Clyde National Health Service Endowment Fund (research funding). D.A.I. participated in the Translational Research Training in Hematology course (run jointly by ASH and EHA). M.C. is a clinical senior lecturer funded by the Chief Scientist Office, Scotland, the Scottish Funding Council, and Leukemia and Lymphoma Research.
Authorship
Contribution: D.A.I. wrote and revised the manuscript; and M.C. revised the manuscript and checked the final version.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Mhairi Copland, Paul O'Gorman Leukaemia Research Centre, College of Medical, Veterinary and Life Sciences, University of Glasgow, Gartnavel General Hospital, 1053 Great Western Road, Glasgow G12 0ZD, United Kingdom; e-mail: mhairi.copland@glasgow.ac.uk.