Evidence suggests that multiple myeloma cells are constantly invading new regions within the bone marrow through induced systemic re-circulation. In this issue of Blood, Azab and colleagues demonstrate that regional bone marrow hypoxia promotes the dissemination of myeloma cells in a manner similar to solid tumor metastasis. This spread is mediated by a hypoxia-induced epithelial-to-mesenchymal cell transition (EMT)–like phenotype.1
Multiple myeloma is an exclusively bone marrow–localized malignancy generating from normal plasma cell differentiation. Plasma cell maturation involves migration of pre-germinal center (GC) B cells from the bone marrow to secondary lymphoid organs and return to the bone marrow as mature plasma cells. Post-GC homing is mediated by CXCR4-induced homing to CXCL12/SDF-1–rich regions of bone marrow niche. Within the bone marrow plasma cell adherence to ECM, bone marrow stromal cells (BMSCs) and other juxtaposed cells lead to the production of crucial factors for bone marrow homeostasis. Unlike their normal counterparts, myeloma cells benefit from the normal effectors within the bone marrow niche, and also hijack and contribute to the environment promoting tumorigenesis, altered bone metabolism, neovascularization, drug resistance, and as now shown, myeloma metastasis.1 The expansion of plasma cells and aberrant neovascularization promotes localized hypoxic subniches.1 Studies in both solid and hematopoietic models suggest that hypoxia contributes directly to cancer survival, migration, and metastasis.2,3 The effect of reduced tissue oxygen is primarily mediated by hypoxia inducible factors (HIFs), a family of heterodimeric basic helix-loop-helix transcription factors consisting of an oxygen sensitive α subunit (HIF-1α, HIF-2α, and HIF-3α) and a constitutively expressed β subunit (HIFβ). HIFα subunits are rapidly degraded under normoxic conditions via a von Hippel-Lindau–dependent ubiquitin-proteosome cascade. Under hypoxic conditions the α subunits stabilize facilitating translocation to the nucleus, heterodimerization with β subunits, and transcriptional activity.
Within solid tumors regional hypoxia exists due to chaotic vasculature, poor oxygen effusion, irregular blood flow, and tumor necrosis.2,4 Intratumoral hypoxia and stabilization of HIFα subunits initiates an adaptive transcriptional program inducing epithelial cells to acquire a mesenchymal cell phenotype termed EMT.2,4 EMT is a highly conserved process integral in embryogenesis, normal tissue development, response to injury, organ fibrosis, as well as critical events in solid tumor invasion, metastasis, and the acquisition of stem cell–like properties.1,2,4,5 EMT-triggering signal pathways involve TGF-β1 and Notch1 as well as the transcription factors SNAIL1, TWIST1, SLUG/SNAIL2, SIP1, ZEB1, and FOXC2, among others.1,2,5 A major biologic consequence of these transcriptional events is the repression of the cell adhesion molecule E-cadherin and cellular release from confines of the local microenvironment.2,4
In multiple myeloma the bone marrow microenvironment promotes proliferation and resistance to chemotherapy. As such, it has been proposed that the bone marrow microenvironment may be a target for new therapeutic agents in the treatment of myeloma.6,7 Supporting this idea, Ghobrial and colleagues have previously demonstrated that targeting of CXCR4 with AMD3100-altered myeloma homing to the bone marrow, increased circulating myeloma cells, and increased sensitivity to cytotoxic agents.8,9 These and other studies examining the CXCL12/CXCR4 axis have resulted in ongoing clinical trials. In addition, these studies indicated that myeloma cells are not statically confined to the bone marrow. Instead, populations of myeloma cells are migrating from one region of the bone marrow to another. As such, myeloma cells “invade” and “metastasize” to new sites of bone marrow. Azab et al hypothesized that this migration was induced by hypoxia associated with progression of disease burden in a manner similar to that of solid organ tumors. Azab et al describe a novel mechanism by which increasing bone marrow tumor burden results in regional hypoxia, inducing dissemination of multiple myeloma cells into peripheral circulation via a hypoxia-induced EMT–like phenotype. Consistent with the EMT phenotype, loss of the E-cadherin correlated with increased expression of SNAIL1, FOXC2, and TGF-β1 and decreased adhesion to BMSCs.1 Together these data suggest that under hypoxic conditions multiple myeloma cells undergo an adaptive transcriptional response in a manner similar to embryonic cells and solid tumor cell metastasis.
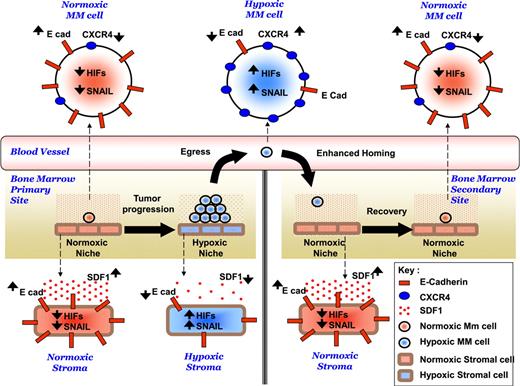
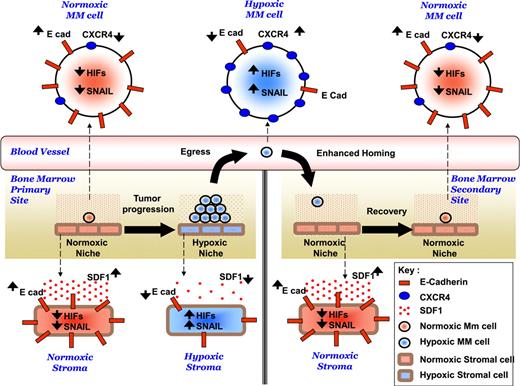
To determine the mechanism mediating extravasation of circulating myeloma cells Azab et al examined CXCR4 under hypoxic conditions. Hypoxia has been shown to induce CXCR4 expression in myeloma cells.10 Consistent with these findings a direct correlation among hypoxia, expression of CXCR4, and chemotaxis of myeloma cells to CXCL12/SDF-1 was identified. In vivo studies demonstrated a CXCR4-dependent increase in the rate of myeloma cell extravasation under hypoxic conditions. Together, these results indicate that regional hypoxia induces (1) an EMT-like transcriptional program modulating myeloma cell egress from the confines of the bone marrow niche via repression of E-cadherin and (2) subsequent re-entrance (metastasis?) to relatively normoxic sites of bone marrow via CXCR4 (see figure).
Hypothesized mechanism of role of hypoxia in the dissemination of MM. Tumor progression induces hypoxia in the MM cells and other cells in the BM microenvironment. Hypoxia activates EMT-related machinery in MM cells and stromal cells, including activation of HIFs, activation of SNAIL, and decreased expression of E-cadherin, which leads to decreased adhesion of MM cells to the BM, decreased SDF1α secretion from stroma, and enhanced egress of MM cells to the circulation. In parallel, hypoxia increases the expression of CXCR4, and consequently increases the migration and homing of MM cells in to the BM to form metastasis to new BM niches. Taken from Figure 8 in the article by Azab et al that begins on page 5782.
Hypothesized mechanism of role of hypoxia in the dissemination of MM. Tumor progression induces hypoxia in the MM cells and other cells in the BM microenvironment. Hypoxia activates EMT-related machinery in MM cells and stromal cells, including activation of HIFs, activation of SNAIL, and decreased expression of E-cadherin, which leads to decreased adhesion of MM cells to the BM, decreased SDF1α secretion from stroma, and enhanced egress of MM cells to the circulation. In parallel, hypoxia increases the expression of CXCR4, and consequently increases the migration and homing of MM cells in to the BM to form metastasis to new BM niches. Taken from Figure 8 in the article by Azab et al that begins on page 5782.
It appears that although labeled a bone marrow–resident malignancy, subpopulations of myeloma cells are leaving the marrow, circulating, and re-entering at distant regions of the marrow. Here, Azab et al demonstrate a novel environment-mediated transcriptional program akin to EMT modulating myeloma cell egress and extravasation. To date, this has been the exclusive domain of embryonic development, response to injury, and solid-tumor cancer metastasis. The results suggest that myeloma cells (and potentially all tumor cells) are subject to differentiation (or de-differentiation) programs induced by the tumor microenvironment. Azab and colleagues demonstrate that the effects of regional hypoxia are not limited to myeloma cells. BMSCs are also subject to the influence of hypoxia. This hypoxia-induced EMT-like phenotype highlights the impact of the bone marrow niche–specific characteristics on disease progression, survival, drug resistance, and now dissemination of myeloma.
The observations raise a number of questions. Current dogma states the myeloma cells require the support of the bone marrow niche. This study demonstrates that hypoxia induced the egress of myeloma cells from the marrow. Do these circulating cells represent a drug-resistant or drug-sensitive population? The extramedullary survival suggests a hypoxia-induced resistant phenotype. Will effectors of EMT phenotype and hypoxia provide new targets for therapeutic intervention? Agents are currently under development that target areas of hypoxia such as the hypoxia-activated pro-drug TH-302.4 However, further work elucidating the effects of EMT on myeloma cells will be needed to determine whether this program represents a viable target. Commonalities have been observed between EMT and cancer stem cells in solid tumors.5 The observation of induced differentiation under hypoxic conditions provides a basis for additional adaptive transcriptional programs and biologic events, including but not limited to, myeloma progenitor development. Lastly, although the report by Azab and colleagues focuses exclusively on the plasma cells disorder multiple myeloma, these data suggest that all tumor cells have a capacity for induced differentiation (de-differentiation) as a result of a well-conserved, inducible program from early development.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■