Abstract
Abstract 1124
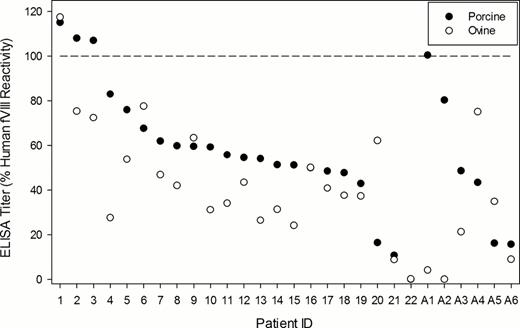
Hemophilia A is an X-linked recessive disorder caused by deficiencies or functional defects in coagulation factor VIII (fVIII). Approximately 20–30% of patients with severe hemophilia A develop antibodies against fVIII (inhibitors) following fVIII replacement therapy, which presents significant complication to the control of subsequent bleeding episodes. State of the art treatment options for patients with inhibitors include fVIII-bypassing agents such as recombinant factor VIIa or activated prothrombin-complex concentrate. Previously, plasma-derived porcine fVIII was a treatment option for inhibitor patients and was effective due to the reduced antigenicity of porcine fVIII toward anti-human fVIII inhibitors. However due to concerns regarding viral contamination, the plasma-derived porcine fVIII products were discontinued and no alternative fVIII products have been made available to patients with inhibitors. Presently, a recombinant porcine fVIII product (OBI-1, Inspiration Biopharmaceuticals) is being investigated in two phase 3 clinical trials for congenital and acquired hemophilia A. Rationale for the development of such a product consists of the prior success of plasma-derived porcine fVIII and the concept that the most effective and lowest risk treatment for fVIII deficiency, even in the presence of inhibitors, remains a fVIII product. Recently, a line of hemophilia A sheep was reestablished from banked frozen sperm and the ovine fVIII (ofVIII) gene, causal mutation, and protein were genetically and biochemically characterized. B-domain deleted (BDD) ovine fVIII shares 86% identity to human fVIII at the amino acid level and confers phenotypic correction, in vivo, to hemophilia A mice using a tail transaction bleeding model. Recombinant ofVIII was expressed in baby-hamster kidney cells and purified to > 95% homogeneity using a two-step ion exchange chromatography procedure. Highly purified ofVIII displays a specific activity of 18,300 units/mg, which is approximately twice that of recombinant BDD human fVIII. Furthermore, the decay of ofVIII activity following thrombin activation is slower than BDD human fVIII suggesting prolonged activity in vivo. Lastly, ofVIII demonstrates equivalent binding to human von Willebrand factor at physiological concentrations in vitro. A translational aim of the present study was to test the hypothesis that unique sequences within ofVIII confer differential antigenicity compared to human and/or porcine fVIII in congenital and acquired inhibitor patient plasmas. To address this hypothesis, the reactivity of 28 samples (22 congenital patient samples designated 1–22, and 6 acquired hemophilia A patient samples designated A1-A6) from the Emory IRB approved inhibitor bank towards recombinant BDD human, porcine, and ovine fVIII were assessed by enzyme-linked immunosorbant assay (Figure 1). When normalized to the reactivity towards human fVIII, the data revealed reduced reactivity towards ofVIII in 27 of 28 total samples. In only one patient was the reactivity towards ofVIII greater than that towards human fVIII and, in this sample, the reactivity towards porcine fVIII also was greater than 100%. Furthermore, plasma reactivity to ovine fVIII was significantly reduced compared to porcine fVIII (P = 0.025; Mann-Whitney U Test). Median values of the relative cross reactivity towards porcine and ovine fVIII were 54 and 38%, respectively. Preliminary inhibitor analysis (Bethesda assay) of three samples shown to contain titers against human fVIII of 25, 19, and 68 BU/ml, revealed undetectable inhibitor titers towards ofVIII in 2 samples, and a titer of 5 BU/ml in the third, respectively. These results suggest that additional orthologous recombinant fVIII molecules may be enabling to the treatment of patients harboring pathogenic inhibitors to human fVIII.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.