Abstract
The number and type of lymphocytes and monocytes/macrophages detectable in the peripheral blood and the lymph nodes of patients with Hodgkin and non-Hodgkin lymphomas has been recently extensively investigated and interesting results indicate they may possibly affect the pathogenesis and prognosis of these diseases. Recent results indicate that the lymphocyte/monocyte ratio (LMR), when assessed at diagnosis by a simple automatic blood count, may predict the clinical outcome of diffuse large B cell lymphoma patients (DLBCL) treated with the R-CHOP chemotherapy program (Li Z-M et al.: PLoS ONE 7(7):2012). The main objective of our study was to evaluate whether: a) the prognostic value of LMR could be confirmed either in patients treated with CHOP and Rituximab (R-CHOP) as well as in those treated with CHOP alone and b) the LMR could improve the prognostic profile as defined by the International Prognostic Index (IPI).
We retrospectively reviewed the clinical outcome of 973 DLBCL patients treated (549 with R-CHOP) and regularly followed at our institutions from 1984 to 2012. The median age of this patients cohort was 61 years (range, 18–86), the Male/Female ratio 55% and the median follow up 44 months (range, 2 – 330). According to the IPI score, 61% of patients were in the low (0–2) risk group, while 39% were in the intermediate or high-risk groups (3–5). A receiver operating characteristic (ROC) curve analysis was used to illustrate in our data set the best cut off values of peripheral blood lymphocyte absolute count (ALC), monocyte absolute count (AMC) or LMR. The relationship between IPI and the LMR was analyzed by the Fisher exact test. Univariate analysis to evaluate differences between variables was performed by the log rank. A multivariate analysis was performed by Cox proportional-hazards models.
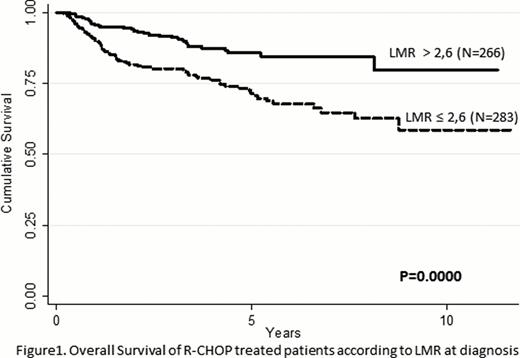
A preliminary ROC curve analysis performed on all patients (treated with or without rituximab) failed to identify any meaningful relationship between Overall Survival (OS) and the ALC, the AMC or the LMR. However, when the same analysis was restricted to patients treated with R-CHOP, we could confirm not only the positive correlation between ALC and AMC and OS, but most importantly that a LMR value >2.6 is the most sensitive (70%) and specific (53%) cut off to predict the OS. Within the R-CHOP treated cohort (N=549), we further investigated the relationships between LMR and the most relevant clinical features measured at diagnosis. Patients with a LMR ≤ 2.6 (52%) had a worst ECOG PS (p= 0.000), a higher LDH level (P= 0.000), a higher IPI (p= 0.000) and more frequently they were male (p= 0.02) and had an advanced Ann Arbor disease stage (p= 0.002). On the contrary, no statistical correlation was observed with age and the presence of extranodal sites. The proportion of patients achieving a complete response or a very good partial response was 95% in patients with a LMR >2.6 and 87% for those with a LMR ≤ 2.6 (p=0.018). More interestingly, among patients failing to achieve CR the proportion of those with a LMR ≤ 2.6 was 79% as compared to 21% among those with a LMR >2.6. The Event Free Survival of patients with a LMR >2.6 was significantly better when compared to those with a LMR ≤ 2.6 (71% vs. 59% at 5 years, p= 0.01) while no difference was observed for the Disease Free Survival. By univariate and multivariate analysis we could show that, similarly to a high IPI, a LMR ≤ 2.6 strongly predict a poor OS (p= 0.0000) (Figure 1). In addition, we could demonstrate a strong interaction between IPI and LMR since patients with a high IPI and LMR ≤ 2.6 are characterized by a very poor prognosis when compared to all the others (p= 0.000).
Our results confirm that a LMR ≤ 2.6 when assessed at diagnosis by a simple automatic blood count is not only a strong predictor of poor survival but it may help to better define a very poor prognostic subgroup in R-CHOP treated DLBCL. This novel prognostic marker is irrelevant when applied to patients receiving chemotherapy alone, giving further support to the notion that lymphocytes and/or monocytes play a crucial role on the therapeutic activity of Rituximab.
Rambaldi:Hoffman-La Roche: Consultancy, Honoraria. Ladetto:Hoffman-La Roche: Consultancy, Honoraria. Gianni:Hoffman-La Roche: Consultancy, Honoraria. Tarella:Hoffman-La Roche: Consultancy, Honoraria.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.