Abstract
Abstract 1566
Response-tailored management of PMLBCL is a major challenge in everyday practice, mostly due to the persistence of post-treatment residual masses of uncertain nature. PET/CT is now widely used in the definition of response and as a prognostic indicator, in Hodgkin lymphoma (HL) and diffuse large B cell lymphoma (DLBCL), while its role in patients with PMLBCL remains to be defined.
The IELSG-26 study was designed to prospectively evaluate the clinical role of PET/CT after rituximab and anthracycline-containing immunochemotherapy (R-CHT) in patients with PMLBCL.
Between January 2007 and July 2010, 125 patients (pts) with PMLBCL were enrolled in 21 institutions and treated with R-CHOP-like (20 pts), R-VACOP-B (34 pts) or R-MACOP-B (71 pts) regimens according to the local policy; consolidation with mediastinal involved field radiotherapy (IFRT) as indicated by local guidelines was allowed. PET/CT scans were planned at baseline, at 3–4 weeks after R-CHT and at 12 weeks after radiotherapy. Central PET/CT review was performed at the end of treatment using the Deauville score (Meignan et al. Leuk Lymphoma 2009) and complete response (CR) was defined as a negative PET scan or one having minimal residual uptake lower than mediastinal blood pool (MBP) activity in regions which were FDG-PET positive at baseline according to the criteria of the International Harmonization Project in Lymphoma (Juweid et al. JCO 2007).
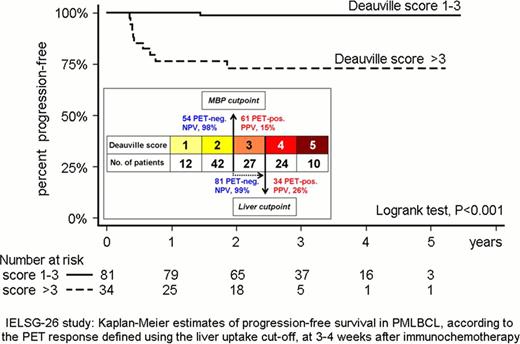
Treatment was administered as initially planned in 119 pts (including IFRT in 106); there were 6 early withdrawals (4 with early progression and 2 with stable disease receiving second-line chemotherapy). PET imaging was not done (n=2) or not evaluable due to technical problems (n=2) in 4 pts, therefore, central review of PET/CT was possible in 115/119 patients. PET/CT visual assessment at 3–4 weeks post-R-CHT showed metabolic CR in 54/115 patients (47%; 95% CI, 36%–56%): in 12 cases (10%; 95% CI, 6%–18%) PET/CT scan was completely negative (score 1 according to the Deauville criteria), while in 42 (37%; 95% CI, 28%–46%) there were small residual masses with an uptake less than MBP (score 2). PET/CT scans showed a positive residual mass after R-CHT in 61/115 pts (53%; 95% CI, 44%–62%). The residual uptake was higher than MBP but below the liver uptake (score 3) in 27 pts (23%; 95% CI, 16%–32%), slightly higher than the liver uptake (score 4) in 24 pts (21%; 95% CI, 14%–29%) and markedly higher than the liver uptake (score 5) in 10 pts (9%; 95% CI, 4%–15%). Despite only 47% of patients attaining a CR -defined by the uptake below MBP activity- after R-CHT, at a median follow-up of 2.8 years, the estimated 5-year overall survival (OS) and progression-free survival (PFS) rates were 96% (95% CI, 89%–98%) and 91% (95% CI, 84%–95%), respectively. The achievement of a CR at 3–4 weeks after R-CHT predicted a longer PFS (p=0.015) with high sensitivity but poor specificity (negative predictive value of 0.98 but positive predictive value of only 0.15) and showed a borderline impact (p=0.052) on OS. Patients with Deauville score 3 had a clinical outcome identical to that of ‘PET negative’ (score 1–2) pts and ROC analysis suggested that moving the cut-point for the definition of CR from the MBP to the liver uptake, will increase specificity while maintaining sensitivity. Indeed, defining the response using the liver uptake as a cutpoint is a better predictor for both PFS (p<0.001) and OS (p=0.001); of 10 pts with disease progression, 9 had score 4–5 and one score 2. The latter was one of the five pts with score 1–3 who were not irradiated. All the 4 recorded deaths occurred in the group of patients with score 4–5.
Using the MBP cut-point, the PET-positive rate (Deauville score>2) after R-CHT in PMLBCL was higher (53%) than in DLBCL. However, more than 90% of pts are projected to be alive and progression-free at 5 years post treatment and a negative PET/CT after R-CHT is significantly associated with a longer PFS. Pts with score 4 and 5 had a significantly worse PFS and OS. Hence, the liver uptake may represent a more appropriate cut-point than MBP to identify poor-risk pts who may need early intensification of therapy. The frequent use of IFRT in this study precludes any clear conclusion about its role, but the new IELSG-37 randomized trial will assess whether mediastinal irradiation can be safely omitted in PMLBCL pts achieving a CR after R-CHT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.