Abstract
Abstract 1702
Prognostic assessment has a crucial role in clinical evaluation of patients (pts) affected by myelodysplastic syndrome (MDS). Recently a Revised International Prognostic Scoring System (IPSS-R) has been developed (Greenberg et al, 2012) to improve the standard IPSS (Greenberg et al, 1997): it identifies five different prognostic categories mainly based on stratification of cytogenetic risk. Another prognostic score proposed in clinical practice is WPSS, based on transfusion dependency and WHO morphologic classification (Malcovati et al, 2005) subsequently modified (rWPSS) introducing level of hemoglobin in lieu of the previous not well defined variable of transfusion dependency (Malcovati et al, 2011).
Aim of our study was to evaluate in a cohort of MDS pts enrolled in the Multiregional Italian MDS Registry the prognostic value of IPSS-R respect to IPSS and compare it with both WPSS and rWPSS.
Among the 1918 MDS pts enrolled in the Multiregional Italian MDS Registry from 1999 to 2012 we excluded all the cases already included in the IWG-PM database that generated the IPSS-R. We thus obtained a cohort of 646 pts with complete follow up. We evaluated the prognostic power of IPSS-R respect to IPSS, WPSS and rWPSS respectively by Harrell's C statistics, analyzing as endpoints overall survival (OS), leukemic evolution (LE) and progression free survival (PFS). For LE we considered leukemic evolution as an event, while all the other causes of death were competing events. For PFS we consider either leukemic evolution or death for any causes as an event.
Median age of MDS patients was 75 years (interquartile range: 69–80 years). 378 (59%) out of 646 pts were males. WHO classification was as follows: 33% RCMD, 10% RAEB-1, 9% RAEB-2, 6% CMML, 2% MDS-U, the remaining 40% were RARS, RA, isolated 5q deletion. Median follow up of censored pts was 17 months.
According to IPSS score, 47% of pts were low risk, 39% Int-1, 10% Int-2 and 4% high risk. WPSS stratification was as follows: 31% were very low (VL) risk, 37% low (L), 19% intermediate (I), 11% high (H) and 2% very high (VH). By applying rWPSS stratification we obtained 30% VL, 35% L, 17% I, 15% H and 3% VH risk pts. IPSS-R risk stratification was as follows: 20% VL, 46% L, 20% I, 9% H and 5% VH risk pts.
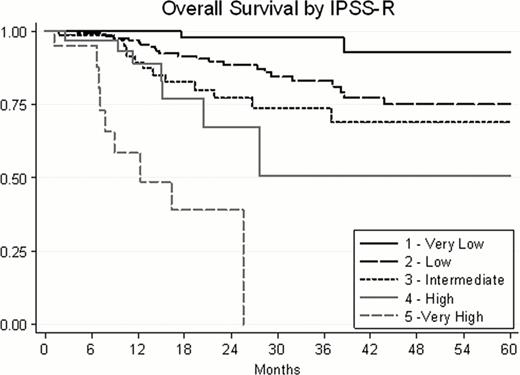
OS was analyzed according to the different scores by Kaplan-Meyer method. All prognostic systems allowed the identification of survival curves with significant differences among the different categories of risk stratification. IPSS-R application defined OS curves which better defined patients prognostic categories as shown in fig 1. In fact Harrel's C statistics demonstrated a better predictive value of the IPSS-R respect to IPSS, but also respect to WPSS and rWPSS (C=0,73; 0,63; 0,65; 0,64 respectively).
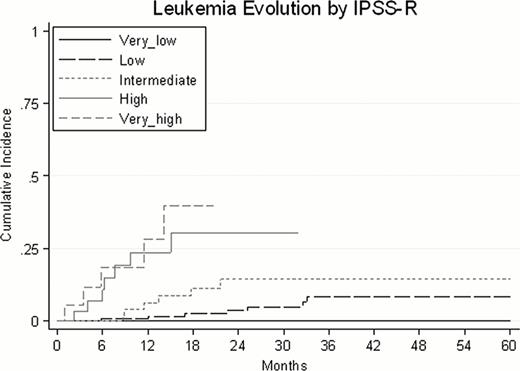
Similar results have been obtained also considering time to LE (fig 2). Harrel's C statistics for LE was 0,84; 0,76; 0,78; 0,77 respectively in IPSS-R, IPSS, WPSS, rWPSS risk stratification groups.
Moreover, we analyzed PFS outcomes (fig 3). Also in this case, IPSS-R showed the greatest prognostic power: Harrel's C statistics was 0,76; 0,67; 0,66; 0,69 respectively in IPSS-R, IPSS, WPSS, rWPSS risk stratification groups.
In our hands, IPSS-R score demonstrated a better prognostic power respect to previously published prognostic systems (IPSS, WPSS, rWPSS). The cohort of MDS patients we employed to validate the new prognostic scoring system has a short follow up (17 months), due to the exclusion of cases already used to establish the IPSS-R system, and the majority of these are lower risk ones. We can conclude that a careful classification based on cytogenetic examination improve the prognostic power of the score. Thus, IPSS-R is confirmed to be a refined tool, easily applicable in real life and empowered respect to the currently used scores to define MDS patient prognosis.
Saglio:Bristol-Myers Squibb: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.