Abstract
Abstract 2034
Mantle cell lymphoma (MCL) is aggressive B-cell neoplasm diagnosed predominantly among elderly men. (R)CHOP-like schemes are effective in remission induction, but the progression-free survival is disappointingly short (median 16–20 months) with median overall survival of 3–4 years. Upfront use of high-dose cytarabine (12 g/m2), autoSCT and rituximab at all stages of therapy is the most effective treatment but possible only with patients younger 65 years. Decrease in AraC doses to 4 g/m2 per cycle significantly reduce progression free survival. Prominent efficacy of gemcitabine-oxaliplatin combinations and irinotecan in relapsed and refractory MCL patients allowed including these drugs in first-line treatment in cases when the scheme R-HD-Met-AraC (Romanguera J. 2005) is impossible.
Toxicity and efficacy assessment of schemes R-DA-EPOCH/R-GIDIOX and R-DA-EPOCH/ R-HD-Met-AraC in primary MCL patients eligible for autoSCT.
Since May 2008 35 untreated MCL patients (median 55 years (29–63), males/females 68,5%/31,5%, MIPIb: 34% low, 26% intermediate, 40% high risk) were enrolled. After first R-EPOCH course (Wilson W. 2003) patients were stratified according to toxicity they had received either R-DA-EPOCH/R-HD-Met-AraC or R-DA-EPOCH/R-GIDIOX. In the absence of hematological toxicity grade 4 for more than 3 days, severe infection complications and signs of renal failure patients underwent treatment under the scheme R-HD-Met-AraC (rituximab 375 mg/m2 day 0, methotrexate 1000 mg/m2 24 hours CI day 1, cytarabine 3000 mg/m2 q 12 hrs days 2–3). If there was one of these complications patients underwent treatment under the scheme R-GIDIOX (rituximab 375 mg/m2 day 0, gemcitabine 800 mg/m2 days 1 and 4, oxaliplatin 120 mg/m2 day 2, irinotecan 100 mg/m2 day 3, dexamethasone 10 mg/m2 IV days 1–5, ifosfamide 1000 mg/m2 days 1–5). Further these courses are rotated: either R-DA-EPOCH/R-HD-Met-AraC or R-DA-EPOCH/R-GIDIOX. Depending on the terms of response, patients received 6–8 courses (3–4 cycles) of chemotherapy and autoSCT (BEAM-R) with in vivo purging by rituximab before harvest and reinfusion. Patients with residual tumor after autoSCT were consolidated with local radiotherapy. Rituximab maintenance was performed every three months for 3 years. The protocol was approved by the local ethics committee. Patients were analyzed in an intent-to-treat basis. Overall survival (OS) and event-free survival (EFS) rates were estimated (± standard error) by using the Kaplan-Meier method. Efficacy of the therapy was assessed by Cheson's response criteria (2008). Toxicity assessment was performed 93 R-DA-EPOCH, 60 R-HD-Met-AraC and 46 R-GIDIOX courses.
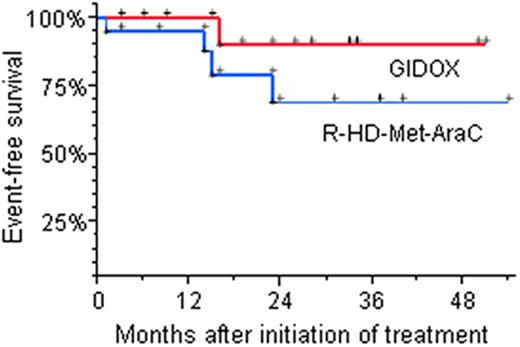
A median follow-up is 23 months (range 3–54). Toward August 2012 26 patients underwent autoSCT: 14 from R-HD-Met-AraC arm and 12 from R-GIDIOX arm. 1 induction death after first HD-Met-AraC course (acute renal failure and septic shock). Maintenance therapy with rituximab was completed in three patients. All patients achieved CR in R-HD-Met-AraC arm. In R-GIDIOX arm OR was 100%: 11 CR and 1 PR (without progression for 26 months after autoSCT). Main non-hematological toxicity of R-GIDIOX was hepatic, with elevated aminotransferases grades 1–2 and 3–4 in 59,5% and 7,1% of courses respectively, without clinical signs. The sources of stem cells were PB in 23 patients and BM in 3 cases of harvest failure after R-GIDIOX. Hematological toxicity of R-GIDIOX course: leukopenia grade 4 was in 71,4% (medium duration was 5,4 days, range 1–13), thrombocytopenia grade 4 was in 42,9%. The estimated 4-years OS rates for the R-GIDIOX group and the R-HD-Met-AraC group were 100% and 68% ± 17%. The estimated 4-years EFS rates for the R-GIDIOX group and the R-HD-Met-AraC group were 90% ± 10% and 69% ± 14%.
Our main goal was to incorporate intensive induction, autoSCT and rituximab maintenance in first line therapy MCL patients. However, HD-Met-AraC scheme is highly toxic and its use is possible only in 2/3 of patients younger 65 years. R-GIDIOX scheme is less toxic than R-HD-Met-AraC and equally effective in response induction and mobilizing, so it could be recommended for those in whom high-dose AraC and methotrexate can potentially cause severe adverse consequences. Such an integrated approach might lead to a shift of paradigm of MCL from an incurable to a curable lymphoma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.