Abstract
Abstract 3257
In previous studies with deferasirox (Exjade®), some patients experienced dose-dependent, non-progressive increases in serum creatinine, mostly within normal limits and mostly reversible with dose reduction/interruption. Although the cause of these increases is not fully understood, the most likely mechanism is hypothesized to be a reduction in glomerular filtration rate (GFR) as a result of a pharmacological effect of deferasirox on the kidney, specifically on its intraglomerular hemodynamics (Schetz et al. 2005). This study was initiated to test this hypothesis and estimate the long-term effect of deferasirox 30 mg/kg/day on renal hemodynamics by measuring changes in renal function markers, specifically GFR, renal plasma flow (RPF) and filtration fraction (FF), in β-thalassemia patients with transfusional iron overload.
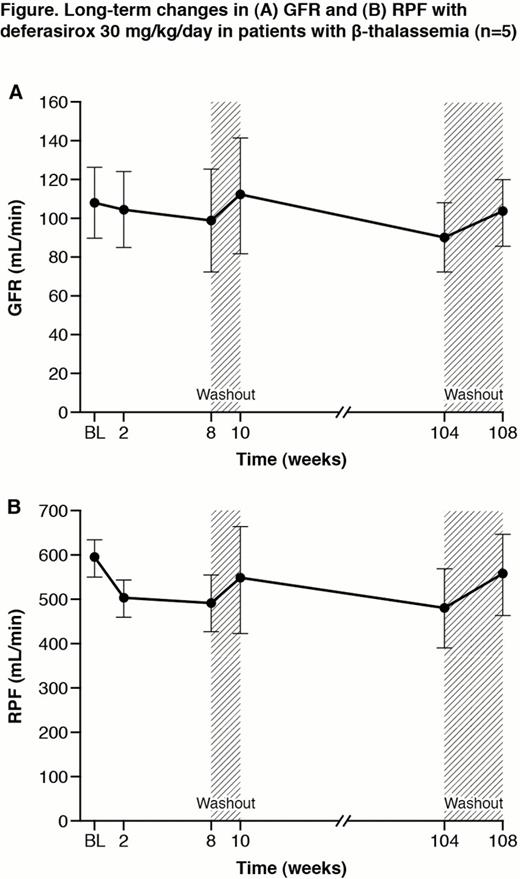
This study enrolled deferasirox-naïve β-thalassemia patients aged ≥18 yrs receiving transfusions every 2–5 wks (iron intake ≥0.25 mg/kg/day), transfusion history ≥20 units packed red blood cells and serum ferritin ≥500 ng/mL or liver iron concentration (LIC) ≥2 mg Fe/g dry weight (dw). Patients were excluded if they had serum creatinine >upper limit of normal (ULN), estimated creatinine clearance (CrCl) <60 mL/min, urinary protein:creatinine ratio >0.5 mg/mg, ALT >5 × ULN, history of nephrotic syndrome, or treatment with drugs known to affect renal parameters. As per the initial protocol, patients received deferasirox 30 mg/kg/day for 8 weeks, followed by a 2-week washout. In order to provide long-term data the study was amended: following the initial 10-week period, patients could receive deferasirox for an additional 94 weeks (up to Week 104) followed by a 4-week washout. GFR and RPF were measured using chromium-labeled ethylenediaminetetraacetic acid (51Cr-EDTA) and 123ortho-iodohippurate (123I-OIH). Parameters were assessed at baseline, 2, 8, 10, 104 and 108 weeks.
Eleven patients were enrolled (mean age 35.2 yrs; 7:4 male:female). For these 11 patients at baseline, median serum ferritin was 2110 ng/mL (range 840–3131 ng/mL); mean LIC 7.3 ± 4.0 mg Fe/g dw. Mean GFR (111.5 ± 17.5 mL/min), RPF (603.5 ± 94.3 mL/min) and FF (0.2 ± 0.03) were normal. Ten patients completed 10 weeks of treatment (one discontinued due to voluntary withdrawal). Five of these patients did not enter the extension trial as they had completed the initial trial prior to the protocol amendment extending the study duration (no patient discontinued due to adverse events [AEs]) and five patients completed the 108-week study.
For the five patients completing the 108-week study, mean GFR decreased from 108.5 ± 18.1 mL/min at baseline to 90.2 ± 17.8 mL/min at Week 104; mean RPF decreased from 595.4 ± 43.1 mL/min at baseline to 479.5 ± 87.6 mL/min at Week 104 (a mean relative decrease of 19.6%; Figure). After 4 weeks' washout following the 104-week period, both mean GFR and RPF recovered to near baseline values: from 90.2 ± 17.8 mL/min at Week 104 to 103.5 ± 17.1 mL/min at Week 108 and from 479.5 ± 87.6 mL/min at Week 104 to 553.5 ± 91.8 mL/min at Week 108, respectively. Mean percentage change for GFR from baseline was –9.5% at Week 8, +2.1% at Week 10, –17.2% at Week 104, and –4.5% at Week 108. For RPF, mean percentage change from baseline was –17.8% at Week 8, –9.0% at Week 10, –19.6% at Week 104 and –7.3% at Week 108. Mean FF showed only mild fluctuations (0.18–0.21) during the study. Serum creatinine was 61.5 ± 15.1 μmol/L at baseline, 65.4 ± 15.1 μmol/L at Week 104 and 62.9 ± 10.7 μmol/L at Week 108; CrCl was 115.0 ± 21.3 mL/min at baseline, 107.4 ± 13.8 mL/min at Week 104 and 109.9 ± 8.8 mL/min at Week 108.
For the 11 patients enrolled, AEs regardless of study drug relationship were mainly gastrointestinal (diarrhea and upper abdominal pain n=3 each, abdominal pain n=2), pyrexia (n=3), rhinitis (n=3), back pain (n=2), headache (n=2), cough (n=3), oropharyngeal pain (n=3), rash (n=2). There were no deaths or serious AEs.
Deferasirox appears to produce a mild effect on renal hemodynamics, reflected by a decrease in RPF, leading to a decrease in GFR; these effects were reversible after drug interruption over the short and long term. Both mean GFR and RPF recovered to near baseline values after washout, suggesting that renal function is stable with up to 2 years' treatment with deferasirox.
Piga:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding. Cappellini:Novartis: Speakers Bureau. Habr:Novartis: Employment. Wegener:Novartis: Employment. Bouillaud:Novartis: Employment.
Author notes
Asterisk with author names denotes non-ASH members.