Abstract
Abstract 3542
The prognosis of acute promyelocytic leukemia (APL) has improved markedly over the last two decades. Clinical trials have demonstrated excellent survival of patients receiving anthracycline-based chemotherapy in combination with all-trans-retinoid acid (ATRA). It is not clear whether the excellent survival results demonstrated in clinical trials during recent years, also do apply to unselected patients including elderly and frail patients for whom a clinical trial may not be available. In order to investigate survival and death rates in APL over the course of treatment, we conducted a retrospective analysis of survival in 105 consecutive APL-patients diagnosed in Denmark January 2000 through June 2012. Data were retrieved from the Danish National Acute Leukemia Registry which covers 95 – 100 % of all acute leukemia cases diagnosed in Denmark since January 2000 (not including children).
A diagnosis of APL was confirmed in 105 (3.9 %) of 2726 adult patients (age ≥ 15 years) with acute myeloid leukemia (AML) diagnosed in Denmark during the 12½ year period. This corresponds to an incidence rate of 1.53 APL cases per million inhabitants per year. The diagnosis of APL was based upon cytogenetic analysis (performed in 96 (91 %) of cases), and/or interphase FISH (iFISH), and/or RT-PCR in a total of 100 cases. In 5 cases clinical signs and morphological changes in bone marrow were highly suggestive of APL and these cases were, thus, deemed to have APL. Median age at diagnosis of APL was 50 years (range 15 to 83 years) and median leukocyte count was 2.65 (range 0.2 to 99.0 × 109/L).
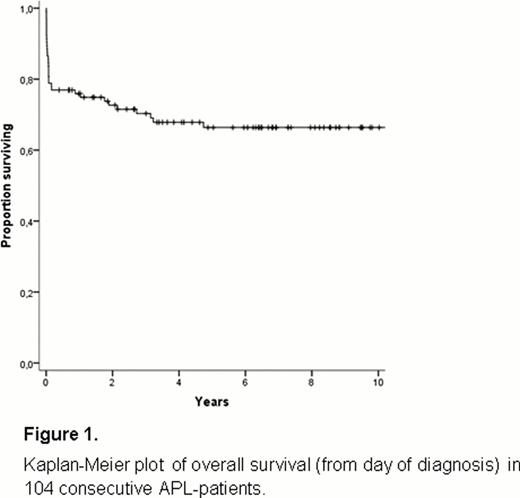
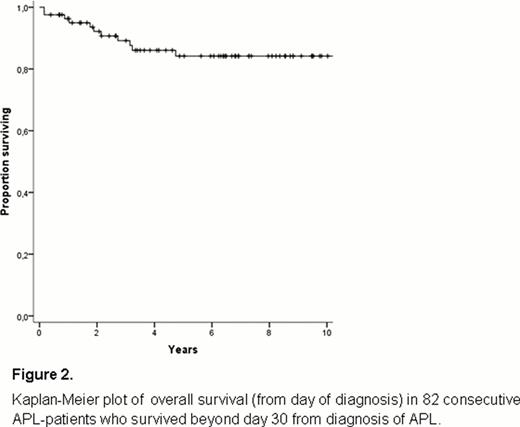
In 104 patients with data available for analysis, very early death (VED, within the first week from the date of diagnostic bone marrow) occurred in 10 cases (9.6 %), and early death (ED, death within 30 day from diagnosis) occurred in 22 (21 %) cases. Death between day 30 and 5 years from diagnosis occurred in 11 cases. No deaths were seen after 5 years from diagnosis. For all patients, estimated overall survival at 10 years was 65 % (Figure 1). Patients surviving beyond day 30 from day of diagnosis (82 cases) had an excellent overall survival of greater than 80 % at 10 years (Figure 2).
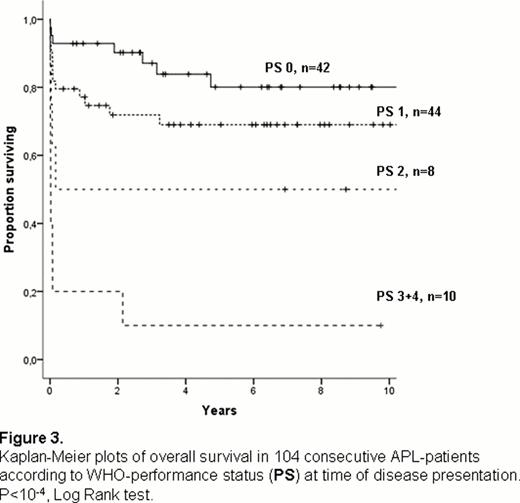
Survival of patients were strongly correlated with WHO-performance status whereas age over 50 years and presenting leukocyte count greater than 10 × 109/L could not be definitely associated with inferior survival (Table 1 and Figure 3).
Factors of importance to survival in unselected APL-patients
| . | Probability of overall survival (Univariate Cox Regression, nevaluable= 104) . | Probability of overall survival (multivariate Cox Regression, nevaluable= 101) . | ||||
|---|---|---|---|---|---|---|
| Variable . | Hazard ratio . | 95% CI of HR . | P value . | Hazard ratio . | 95% CI of HR . | P value . |
| Age (≤50 vs. >50 years) | 2.17 | 1.07–4.42 | 0.03 | 1.44 | 0.67–3.09 | NS |
| WHO performance status (0–1 vs. ≥2) | 5.20 | 2.57–10.5 | < 10−4 | 4.06 | 1.88–8.78 | < 10−4 |
| WBC (≤10 × vs.>10 × 109/L) | 1.76 | 0.86–3.61 | NS | 1.62 | 0.79–3.33 | NS |
| . | Probability of overall survival (Univariate Cox Regression, nevaluable= 104) . | Probability of overall survival (multivariate Cox Regression, nevaluable= 101) . | ||||
|---|---|---|---|---|---|---|
| Variable . | Hazard ratio . | 95% CI of HR . | P value . | Hazard ratio . | 95% CI of HR . | P value . |
| Age (≤50 vs. >50 years) | 2.17 | 1.07–4.42 | 0.03 | 1.44 | 0.67–3.09 | NS |
| WHO performance status (0–1 vs. ≥2) | 5.20 | 2.57–10.5 | < 10−4 | 4.06 | 1.88–8.78 | < 10−4 |
| WBC (≤10 × vs.>10 × 109/L) | 1.76 | 0.86–3.61 | NS | 1.62 | 0.79–3.33 | NS |
From this population-based analysis we conclude that early death continues to be the predominant hazard to patients with APL. Two thirds of deaths in APL-patients do occur during the first month from diagnosis. Patients with a poor performance status at disease presentation carry a particularly dismal prognosis. For all APL-patients, every possible effort should be made to facilitate prompt diagnosis and speedy initiation of treatment with ATRA and anthracycline-based chemotherapy. When timely applied, currently available treatments are highly effective and result in cure in a high proportion of patients including elderly patients and patients with high leukocyte count at time of disease presentation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.