Abstract
Abstract 3810
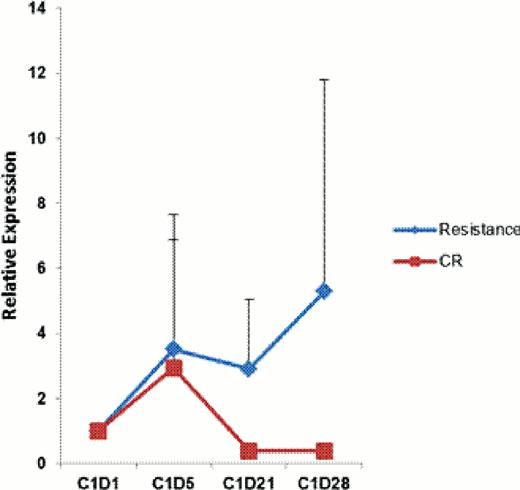
The pathogenesis of MDS is multifactorial including both cell intrinsic alterations, such as mutations, and cell extrinsic stimuli such as inflammatory signals and immune deregulation. It has been postulated that hypomethylating agents exert their effects in part via regulation of expression of cell surface antigens. The prognosis of patients that lose response to HMAs is very poor and the mechanisms of action of resistance to HMAs are not understood. Tumor cells develop multiple resistance mechanisms to escape host immune response and permit tumor cell growth which including T-cell dysfunction. Programmed death-1 (PD-1) is a negative costimulatory receptor on activated T lymphocytes which counters the activation signal provided by T cell receptor ligation. Tumor cells can express PD-1 ligands, PD-L1 and PD-L2, which can induce immunosuppressive T-cells. Recent studies have indicated that demethylation of the locus that encodes PD-1 leads to exhausted CD8+ T cells after chronic virus infection. We hypothesized that PD-1 signaling may be involved in resistance to HMAs. We first evaluated 8 myeloid leukemia cell lines, HL-60, NB4, THP1, U937, ML1, OCI-AML3, HEL and KG1, for expression of PD-1, PD-L1, PD-L2 and CTLA4 (another negative regulator of T-cell activation) by Q-PCR, except OCI-AML3, PD-L1 was detectable in all of these cell lines, whereas CTLA4 and PD-1 can only be detected in KG1. Subsequently, we analyzed the expression of PD-L1 by Q-PCR in CD34+ cells sorted from bone marrow of 129 newly diagnosed MDS patients. Compared with normal CD34+ controls, 38 (29%) of the patients had aberrant up-regulation of PD-L1 RNA expression (folds 2–814). We also analyzed 10 AML CD34+ samples from bone marrow and 3 of them were up-regulated. We then confirmed at the protein level using immunohistochemistry for the expression of PD1 and PD-L1 in 14 AML and 4 MDS bone marrow specimens. We observed that AML blasts were positive for PD-L1 whereas stroma/non-blast cellular compartment were positive for PD-1. We then analyzed the expression level of PD-1, PD-L1, PD-L2 and CTLA4 by Q-PCR in peripheral blood mononuclear cells of a cohort of patients with AML or MDS treated in different clinical trials of epigenetic therapy. These included: 18 patients from a phase 2 trial of vorinostat in combination with azacitidine (which included 11 patients that achieved complete remission (CR) and 7 resistant); 11 patients from a phase 2 study of low dose decitabine (all these patients were resistant to the therapy); 26 patients from phase I/II study of the combination of 5-azacitidine with lenalidomide (which include 5 CR patients and 21 resistant). Prior to therapy, PD-1, PD-L1, PD-L2 and CTLA4 expression was up-regulated in 25 (45%), 23 (42%), 13 (24%) and 5 (9%) of the patients respectively compared to normal peripheral blood mononuclear cells. After a course of therapy 24 (44%), 27 (49%), 20 (36%) and 31 (56%) of the patients acquired induced up-regulated expression of these genes. Of importance, in the group of patients treated with vorinostat in combination with azacitidine, patients resistant to therapy had more signigicant increase of gene expression compared to patients that achieved a CR (Figure 1). To model this observation, we treated KG-1 and THP1 cells with different concentrations of decitabine (0 to 10 uM) and observed a dose dependent up-regulation of PD-L1 and PD-L2 in THP1 cells, and CTLA4, PD-1, PD-L1 in KG1 cells at doses over 0.5 uM. Exposure to decitabine resulted in demethylation of PD-1 in these cell lines. In this study, we demonstrate aberrant expression of CTLA4, PD-1 and PD-1 ligands in MDS and AML patients and that HMAs can up-regulate the expression of these genes, suggesting that PD-1 signaling may be involved in resistance mechanisms to HMAs. Blockade of this pathway can be a potential therapy in MDS and AML.
PD-L1 expression in the group of patients treated with vorinostat in combination with azacitidine.
PD-L1 expression in the group of patients treated with vorinostat in combination with azacitidine.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.