Abstract
Abstract 3930
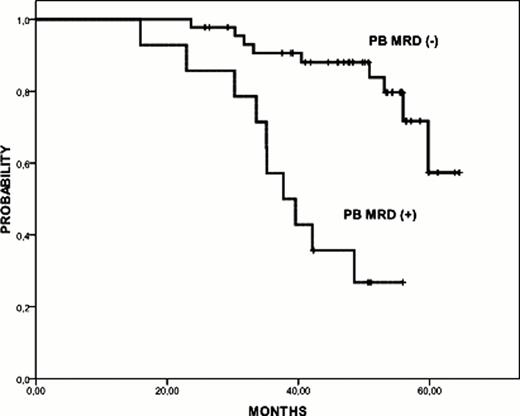
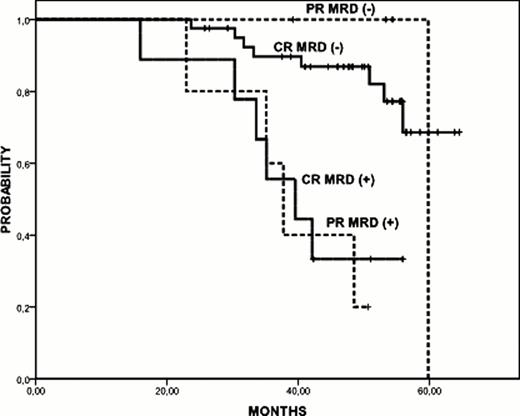
Chemoimmunotherapy combination regimens achieve high rates of negative minimal residual disease responses in CLL, which has been correlated with prolonged PFS and OS. In the present study, we addressed the prognostic value of MRD levels obtained after rituximab, fludarabine, cyclophosphamide, and mitoxantrone (R-FCM) induction treatment in the response duration of patients with CLL included in the GELLC-1 trial and receiving maintenance rituximab treatment (Bosch et al. J Clin Oncol 27:4578–4584, 2009). Patients achieving CR or PR after R-FCM induction received rituximab maintenance consisting of rituximab 375 mg/m2 every three months for two years (up to 8 cycles). MRD was evaluated by four-color flow cytometry assays giving a sensitivity < 10−4 in paired peripheral blood (PB) and bone marrow (BM) samples three months after R-FCM induction therapy, every 6 months during rituximab maintenance, and at the final restaging 3 months after conclusion of treatment. Sixty-seven patients (median age 60 years, 70% male) received a median of 8 cycles of rituximab maintenance (range, 1 to 8), 76% of them completing the entire planned treatment. After R-FCM induction, MRD was considered negative in 45/59 patients (76%) in PB and in 35/63 patients (55%) in BM. Of note, these patients with negative MRD in PB had longer PFS in comparison to those with detectable MRD (at 4 years, 88%, [95%IC 98%-78%] vs 27%, [95%IC 51%-3%] respectively; p<0.01) (Figure 1). MRD negativity in BM showed a trend for a prolonged PFS (p=0.056). When MRD levels in BM after R-FCM induction where categorized, we observed that PFS was similar between the MRD negative (<10−4; n=35) and intermediate (>10−4 to <10−2; n=20) subgroups, whereas it was significantly shorter in patients showing high (>10−2, n=8) MRD levels (PFS at 4 years, 84%, 74%, and 25%, respectively, p<0.01). MRD levels after RFCM induction were compared between PB and BM paired samples. Whereas 12/57 patients (21%) that were MRD negative in PB resulted positive in BM, all patients with negative MRD in BM also had negative MRD in PB. Patients with discrepancies (negative in PB but positive in BM) in their MRD status presented a similar PFS than those with negative MRD in BM (4 year PFS, 85% vs. 90%, P=NS). The impact of MRD levels in PB achieved after R-FCM induction on PFS was also analyzed. MRD status proved to be a superior predictor for PFS than clinical response (Figure 2). In addition, when different prognostic variables (lymphocyte doubling time [LDT, cutoff 12 months], ZAP-70, serum ß2microglobulin and LDH, cytogenetic abnormalities, and MRD levels) were analyzed as predictors for PFS, only MRD status in PB along with LDT remained significantly predictive. After rituximab maintenance, 40.6% of patients achieved a MRD-negative CR, 40.6% a MRD+ CR, 5% a PR, and 14% failed to treatment. Median time to conversion from negative to positive MRD was 45.4 months, significantly longer than that observed in patients treated with FCM only (45.4 vs. 16.4 months; p=0.011) (Bosch et al. Clin Can Res 14:155–161,2008). Moreover, 3 patients that achieved MRD negative in PB but remained MRD positive in BM after the initial R-FCM treatment, became MRD-negative in BM upon rituximab maintenance. Patients that remained MRD negative in PB at the end of rituximab maintenance treatment had an excellent outcome with a PFS of 93% at 4 years in comparison to 68% in patients with MRD positive status (p=0.016). In conclusion, in patients receiving rituximab maintenance MRD levels obtained after R-FCM induction correlated with PFS duration, this correlation being independent of the clinical response attained. The sensitivity of the detection of MRD in these patients was higher in BM than in PB. Finally, maintenance treatment with rituximab seems to prolong the PFS of patients with MRD positive status, minimizing the negative impact of low levels of MRD after induction therapy.
Off Label Use: Rituximab is currently not approved as maintenance therapy for patients with chronic lymphocytic leukemia. Bosch:Hoffman La Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.