Abstract
Abstract 423
Cytogenetic abnormalities at diagnosis are seen in 20–70% of patients with myelodysplastic syndromes (MDS). The International Prognostic Scoring System -revised (IPSS-R) classifies these cytogenetic abnormalities into five prognostic groups: very good (del(11q), ΠY with overall survival (OS) of 61 months); good (normal, del(20q), del(5q), del(12p) with OS 49 months); intermediate (+8,7q-, i(17q),+19,+21 with OS 26 months); poor (der(3)q21/q26, −7, complex with 3 abnormalities with OS 16 months); and very poor (complex with >3 abnormalities with OS of 6 months) (Schanz J, JCO 2012, Greenberg P, Blood 2012). Monosomal karyotype (MK) is defined as the presence of two or more autosomal monosomies or a single monosomy associated with a structural abnormality. We have previously shown that MK identifies a prognostically worse subgroup of MDS patients with a complex karyotype (Patnaik M, Leukemia 2010).
To validate the IPSS-R cytogenetic risk groups in an independent cohort of patients with MDS.
Evaluate the prognostic impact of MK to refine the current IPSS-R cytogenetic risk classification.
The Mayo Clinic database for MDS was used to identify patients in whom bone marrow histologic and cytogenetic information was obtained at the time of diagnosis. WHO criteria were used for MDS diagnosis and leukemic transformation.
i) Patient characteristics: A total of 1,014 patients met the above-stipulated criteria. Median age of the cohort was 71 years (range: 18–98 years) with 684 (67%) males. 819 patients (81%) had primary MDS with 195 cases (19%) of therapy-related MDS. 759 patients (75%) are dead at a median follow-up of 18 months (range: 0–223 months) with leukemic transformation documented in 125 cases (12%). IPSS-R risk distribution was as follows: very low (n=149, 15%), good (n=261, 26%), intermediate (n=221, 22%), high (n=131, 13%), and very high (n=252, 25%).
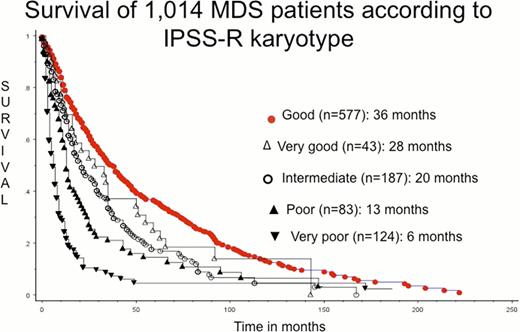
ii) IPSS-R karyotype (Entire cohort; n=1,014): The five cytogenetic groups by IPSS-R were as follows: very good (n=43, 4%), good (n=577, 57%), intermediate (n=187, 18%), poor (n=83, 8%), and very poor (n=124, 12%). We evaluated the prognostic impact of the above groups by Kaplan Meier and Cox proportional hazards analysis. OS for the five cytogenetic groups was as follows: good (36 months), very good (28 months), intermediate (20 months), poor (13 months), and very poor (6 months) (Figure 1). OS of patients with very good karyotype was significantly better than patients with very poor and poor karyotype (p<0.0001, RR 3.2 and p=0.04, RR 1.6 respectively) but similar to patients with intermediate and good karyotype (p=0.22 and 0.28 respectively).
iii) IPSS-R karyotype (Primary MDS; n=819): Cytogenetic risk groups by IPSS-R were as follows: very good (n=38, 5%), good (n=512, 63%), intermediate (n=153, 19%), poor (n=46, 6%), and very poor (n=70, 9%). OS of the five groups was as follows: good (39 months), very good (23 months), intermediate (21.5 months), poor (14.5 months), and very poor (6.5 months). OS of patients with very good karyotype was significantly better than patients with very poor karyotype (p=0.0002, RR 2.5) but similar to patients with poor, intermediate and good karyotype (p=0.23, 0.26 and 0.18 respectively).
iv) Monosomal karyotype: MK was identified in 153 (15%) cases of which 4 cases were intermediate, 42 poor, and 107 very poor by IPSS-R. OS of patients with MK was similar to those with very poor karyotype (6 months). In addition, OS of patients with very poor without MK was akin to patients with poor without MK (p=0.21). Furthermore, among primary MDS we identified 83 (8%) cases of MK of which 4 were intermediate, 21 were poor, and 58 very poor by IPSS-R. We confirmed that OS of patients with MK was similar to patients with very poor karyotype (6.5 months). Moreover, survival of patients with very poor without MK was similar to patients with poor without MK (p=0.51).
In this independent analysis of 1,014 patients with MDS, IPSS-R cytogenetic risk characterization failed to discriminate between very good, good and intermediate prognostic groups. In addition, patients with very poor without MK have a similar prognosis to patients with poor without MK and should be included in the poor category whereas the presence of MK should warrant inclusion into the very poor risk category.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.