Abstract
Abstract 4652
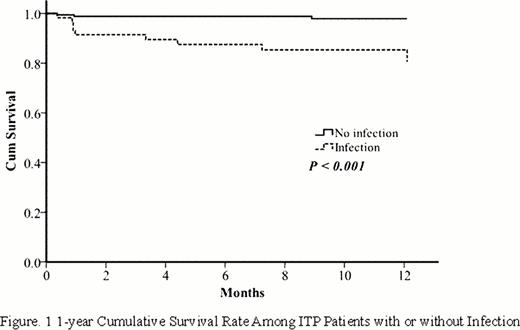
Patient with refractory ITP have increased mortality compared with the normal population. Apart from major bleeding, infection was a major risk of death of these patients.1However, infections after diagnosis of immune thrombocytopenia are less addressed in the literature and its clinical impact on outcome of patients with ITP has not been well-addressed. This study aimed to characterize risk of infection events after diagnosis of ITP and its impact on outcome of these patients. We retrospectively evaluated 239 patients (109 men, 130 women; medium age: 63 yr) diagnosed between Jan 1, 1997 to Aug 31, 2011. Every patient received at least steroid treatment according to platelet count or bleeding symptoms after diagnosis. Infection event occurred in 59 patients (24.7%) within 6 months after diagnosis. Multivariate analysis revealed that age (>65 yr) was the most important risk factor regarding to infection (p=0.048, 95% CI 1.005 to 4.007). 1-year mortality rate after ITP diagnosis was significantly higher in those patients with infection after steroid treatment (p<0.001). We conclude that elderly patients with ITP are more prone to infections which have negative impact on post-diagnosis 1 year survival.
The Demographic and Clinical Characteristics of Patients With Immune Thrombocytopenia
| Patient characteristic . | All patients (n=239) . |
|---|---|
| Sex, no. of patients (%) | |
| Male | 109 (45.6%) |
| Female | 130 (54.4%) |
| Medium age, y | 63.0 (18∼97) |
| Medium follow-up period, months | 19.08 (0.1∼155) |
| Thrombocytopenia1 no. of patients (%) | 195 (81.6%) |
| Severe | 44 (18.4%) |
| Moderate | 20 (8.4%) |
| Evan's syndrome, no. of patients (%) | 19 (7.9%) |
| Splenectomy, no. of patients (%) | 35 (14.6%) |
| Comorbidity, no. of patients (%) | 74 (31%) |
| DM | 12 (5%) |
| HTN | 8 (3.3%) |
| CKD | 12 (5%) |
| CHF | 8 (3.3%) |
| CVA | 96 (40.2%) |
| COPD | 59 (24.7%) |
| Any | 13 (5.4%) |
| Infectious event, no. of patients (%) | 11 (4.6%) |
| Total patient | 2 (0.8%) |
| Mortality, no. of patients (%) | |
| Total numbers | |
| Death due to infection | |
| Death due to bleeding |
| Patient characteristic . | All patients (n=239) . |
|---|---|
| Sex, no. of patients (%) | |
| Male | 109 (45.6%) |
| Female | 130 (54.4%) |
| Medium age, y | 63.0 (18∼97) |
| Medium follow-up period, months | 19.08 (0.1∼155) |
| Thrombocytopenia1 no. of patients (%) | 195 (81.6%) |
| Severe | 44 (18.4%) |
| Moderate | 20 (8.4%) |
| Evan's syndrome, no. of patients (%) | 19 (7.9%) |
| Splenectomy, no. of patients (%) | 35 (14.6%) |
| Comorbidity, no. of patients (%) | 74 (31%) |
| DM | 12 (5%) |
| HTN | 8 (3.3%) |
| CKD | 12 (5%) |
| CHF | 8 (3.3%) |
| CVA | 96 (40.2%) |
| COPD | 59 (24.7%) |
| Any | 13 (5.4%) |
| Infectious event, no. of patients (%) | 11 (4.6%) |
| Total patient | 2 (0.8%) |
| Mortality, no. of patients (%) | |
| Total numbers | |
| Death due to infection | |
| Death due to bleeding |
Moderate thrombocytopenia= platelet counts between 30.0 × 109/L and 100.0 × 109/L; severe thrombocytopenia counts below 30.0 × 109/L.
Clinical Characteristics of Infection Events
| Patient characteristic . | All events (n=70) . |
|---|---|
| Infectious event, no. (%) | |
| Total event | 70 |
| Pneumonia | 31 (44.2%) |
| UTI | 13 (15.6%) |
| Herpes zoster | 9 (12.8%) |
| Cellulitis | 7 (10.0%) |
| Others1 | 10 (14.3%) |
| Pathogens no. of event | |
| Events with definite cultured pathogen | 29 |
| Staphylococcus aureus | 8 |
| Klebsiella pneumonia | 6 |
| Yeast2 | 6 |
| Pseudomonas aeruginosa | 5 |
| Acinetobacter baumannii | 4 |
| Stenotrophomonas maltophilia | 4 |
| E. coli | 3 |
| Enterobacter spp. | 3 |
| Others3 | 5 |
| Infection event date | |
| 1st month | 23 (32.9%) |
| 2nd month | 17 (24.3%) |
| 3rd month | 7 (10.0%) |
| 4th month | 8 (11.4%) |
| 5th month | 6 (8.5%) |
| 6th month | 9 (12.9%) |
| Patient characteristic . | All events (n=70) . |
|---|---|
| Infectious event, no. (%) | |
| Total event | 70 |
| Pneumonia | 31 (44.2%) |
| UTI | 13 (15.6%) |
| Herpes zoster | 9 (12.8%) |
| Cellulitis | 7 (10.0%) |
| Others1 | 10 (14.3%) |
| Pathogens no. of event | |
| Events with definite cultured pathogen | 29 |
| Staphylococcus aureus | 8 |
| Klebsiella pneumonia | 6 |
| Yeast2 | 6 |
| Pseudomonas aeruginosa | 5 |
| Acinetobacter baumannii | 4 |
| Stenotrophomonas maltophilia | 4 |
| E. coli | 3 |
| Enterobacter spp. | 3 |
| Others3 | 5 |
| Infection event date | |
| 1st month | 23 (32.9%) |
| 2nd month | 17 (24.3%) |
| 3rd month | 7 (10.0%) |
| 4th month | 8 (11.4%) |
| 5th month | 6 (8.5%) |
| 6th month | 9 (12.9%) |
Other infection includes oral candidiasis (2), cholangitis (1), fungemia (1), bacteremia (1), intraabdominal abscess (1), facial abscess (1), osteomyelitis (1), pseudomembranous colitis (1), acute suppprative periodontitis (1).
Including Candida albicans and Aspergillus.
Other pathogen including Streptococcus agalactiae (1), Serratia spp (1) Clostridium dificile (1), Chryseobacterium meningosepticum (1), gram positive cocci (1).
Baseline Characteristics of Patients with or without Infection
| Character . | No infection (n=180) . | Infection (n=59) . | p value . |
|---|---|---|---|
| Sex | 0.006* | ||
| M | 73 (40.6%) | 36 (61.0%) | |
| F | 107 (59.4%) | 23 (39.0%) | |
| Age | 0.616 | ||
| Medium | 57 | 73 | |
| Range | 18∼90 | 23∼97 | |
| Thrombocytopenia | 0.268 | ||
| Moderate | 36 (20.0%) | 8 (13.6%) | |
| Severe | 144 (80.0%) | 51 (86.4%) | |
| Evan's syndrome | 14 (7.8%) | 6 (10.2%) | 0.565 |
| Splenectomy | 13 (7.2%) | 6 (10.2%) | 0.468 |
| Cormobidity | |||
| DM | 21 (11.7%) | 14 (23.7%) | 0.023* |
| HTN | 51 (28.3%) | 23 (39.0%) | 0.125 |
| CKD | 6 (3.3%) | 6 (10.2%) | 0.037* |
| CHF | 5 (2.8%) | 3 (5.1%) | 0.393 |
| CVA | 8 (4.4%) | 4 (6.8%) | 0.476 |
| COPD | 4 (2.2%) | 4 (6.8%) | 0.095 |
| Any | 64 (35.8%) | 31 (52.5%) | 0.022* |
| ANC<1000 | 49 (27.2%) | 26 (44.1%) | 0.016* |
| Response1 | 0.001* | ||
| CR+PR | 151 (83.9%) | 38 (64.4%) | |
| NR | 29 (16.1%) | 21 (35.6%) |
| Character . | No infection (n=180) . | Infection (n=59) . | p value . |
|---|---|---|---|
| Sex | 0.006* | ||
| M | 73 (40.6%) | 36 (61.0%) | |
| F | 107 (59.4%) | 23 (39.0%) | |
| Age | 0.616 | ||
| Medium | 57 | 73 | |
| Range | 18∼90 | 23∼97 | |
| Thrombocytopenia | 0.268 | ||
| Moderate | 36 (20.0%) | 8 (13.6%) | |
| Severe | 144 (80.0%) | 51 (86.4%) | |
| Evan's syndrome | 14 (7.8%) | 6 (10.2%) | 0.565 |
| Splenectomy | 13 (7.2%) | 6 (10.2%) | 0.468 |
| Cormobidity | |||
| DM | 21 (11.7%) | 14 (23.7%) | 0.023* |
| HTN | 51 (28.3%) | 23 (39.0%) | 0.125 |
| CKD | 6 (3.3%) | 6 (10.2%) | 0.037* |
| CHF | 5 (2.8%) | 3 (5.1%) | 0.393 |
| CVA | 8 (4.4%) | 4 (6.8%) | 0.476 |
| COPD | 4 (2.2%) | 4 (6.8%) | 0.095 |
| Any | 64 (35.8%) | 31 (52.5%) | 0.022* |
| ANC<1000 | 49 (27.2%) | 26 (44.1%) | 0.016* |
| Response1 | 0.001* | ||
| CR+PR | 151 (83.9%) | 38 (64.4%) | |
| NR | 29 (16.1%) | 21 (35.6%) |
Response: complete response (CR) partial response (PR) no response (NR).
Multivariate Analysis for the Short Term (Within 6 Months) Infection Risk in Patient with ITP
| Dependant variable . | Odds ratio . | P value . | 95% confidence interval . | |
|---|---|---|---|---|
| Lower bound . | Upper bound . | |||
| Age >65 | 2.205 | 0.048* | 1.005 | 4.077 |
| ALC<1000 | 1.807 | 0.066 | 0.961 | 3.399 |
| Any cormobidity | 1.374 | 0.357 | 0.699 | 2.699 |
| Dependant variable . | Odds ratio . | P value . | 95% confidence interval . | |
|---|---|---|---|---|
| Lower bound . | Upper bound . | |||
| Age >65 | 2.205 | 0.048* | 1.005 | 4.077 |
| ALC<1000 | 1.807 | 0.066 | 0.961 | 3.399 |
| Any cormobidity | 1.374 | 0.357 | 0.699 | 2.699 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.