Abstract
Abstract 4837
The tumor microenvironment includes tumor cells, and host-derived endothelial cells, fibroblasts, innate and adaptive immune cells. Tumors may induce neo-vascularization that supports local tumor growth or immune suppression and tolerance that facilitates tumor metastasis. We hypothesized that the patients with higher numbers of circulating CD34+ endothelial progenitor cells (CD34+/CD146+/CD45-, CEC), a cellular bio-marker for vasculogenesis, would have worse post-treatment outcomes and patients with more hematopoietic progenitor cells (CD34+/CD45+/CD45dim/CD133+, HPC) and Immune cells including T-cells would have better outcomes.
We analyzed blood samples from sixty-two patients with advanced NSCLC at 3 time points: before chemotherapy, after cycle one, and at completion of treatment or progression of disease, in an IRB-approved protocol. CEC, HPC, and immune subsets were measured by high throughput multi-parameter flow cytometry, 2.5,000,000 events were acquired using a lyse, no-wash method optimized for rare event detection. Primary outcomes were progression free survival(PFS) and Overall Survival(OS) from the time of study entry. The patient population was stratified into groups based on optimum cut-off point for each cell subset of interest. Statistical analysis was done with log-rank test and Cox regression.
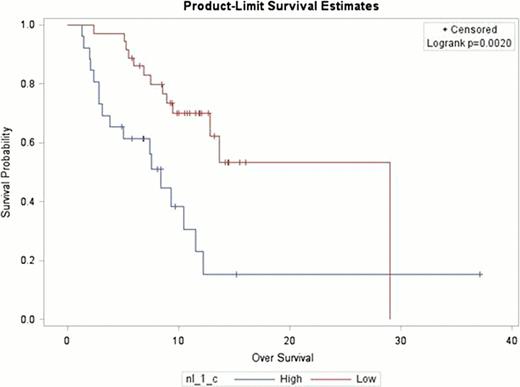
Mean age at diagnosis was 64 (37–87 years), 30 events (death) occurred with median follow-up of 9.3 months. Forty-six patients (74%) had disease progression with a median follow-up of 4.7 months. At baseline lower numbers of WBC, Neutrophil lymphocyte ratio(NLR), CEC, HPC were associated with better PFS, while only WBC and Neutrophil lymphocyte ratio (NLR) were associated with a favorable OS. While lower numbers of Immune cells were associated with worse PFS and OS (increased HR death or relapse) in univariate analysis as noted in the Table. Only covariates that were significant and non collinear were entered in the Multivariable model adjusted for age, gender, smoking, race, TNM stage, pathology, and performance status at diagnosis. This showed that baseline numbers of CD4+ T-cell (HR 0.46; 95% CI 0.33–0.98; p= 0.045), Myeloid DC (HR 0.38; 95% CI 0.39–0.81; p=0.012), HPC (continuous variable) (HR 0.78; 95% CI 0.64–0.93; p= 0.008) were significant for disease progression, while NLR was significant for death after study entry (Figure; HR 3; 95% CI 1.45–6.25; p=0 0.003).
In patients with advanced NSCLC, lower numbers of HPC and NLR were associated with improved PFS and OS respectively. Lower numbers of immune subsets at diagnosis were associated with inferior outcomes to treatment, supporting the role for immune-mediated disease control.
Univariate Analysis
| . | . | Progression Free Survival (HR death or relapse) . | . | Overall Survival (HR death) . | . |
|---|---|---|---|---|---|
| Covariate . | Median number . | HR (95% CI) . | P-value . | HR (95% CI) . | P-value . |
| Metastasis | 2.44 (1.26–4.76) | 0.007 | |||
| Initial PS | 1.96 (1.0–4.0) | 0.049 | |||
| CEC, cells/uL (by 0.02058) | 0.08 | 4 (0.95–16.6) | 0.042 | ||
| HPC, cells/uL (continuous variable) | 0.92 | 0.75 (0.61–0.93) | 0.005 | ||
| CD4 Cell Count, cells/ml (by 480) | 746 | 0.34 (0.17–0.68) | 0.002 | 0.34 (0.16–0.74) | 0.004 |
| WBC, cells/ml (by 6.2) | 8.83 | 2.22 (0.97–5) | 0.054 | 5 (1.16–25) | 0.02 |
| NLR (by 3.8283) | 5.51 | 3.12 (1.61–6.25) | <0.001 | 3.03 (1.44–6.25) | 0.002 |
| Gamma delta T cells, cells/ml (by 17) | 61 | 0.52 (0.27–0.99) | 0.04 | 0.39 (0.18–0.84) | 0.014 |
| Myeloid dendritic cells, cells/ml (by 2.912) | 5.94 | 0.28 (0.13–0.56) | <0.001 | 0.40 (0.18–0.88) | 0.019 |
| Plasmacytoid dendritic cells/ml (by 2.3667) | 2.37 | 0.4 (0.16–1.0) | 0.04 | ||
| B cells, cells/ml (by 70.86) | 187.79 | 0.37 (0.18–0.75) | 0.004 | 0.42 (0.19–0.90) | 0.023 |
| B regulatory cells, cells/ml (by 3.948) | 22.7 | 0.41 (0.20–0.81) | 0.009 | 0.28 (0.13–0.62) | <0.001 |
| . | . | Progression Free Survival (HR death or relapse) . | . | Overall Survival (HR death) . | . |
|---|---|---|---|---|---|
| Covariate . | Median number . | HR (95% CI) . | P-value . | HR (95% CI) . | P-value . |
| Metastasis | 2.44 (1.26–4.76) | 0.007 | |||
| Initial PS | 1.96 (1.0–4.0) | 0.049 | |||
| CEC, cells/uL (by 0.02058) | 0.08 | 4 (0.95–16.6) | 0.042 | ||
| HPC, cells/uL (continuous variable) | 0.92 | 0.75 (0.61–0.93) | 0.005 | ||
| CD4 Cell Count, cells/ml (by 480) | 746 | 0.34 (0.17–0.68) | 0.002 | 0.34 (0.16–0.74) | 0.004 |
| WBC, cells/ml (by 6.2) | 8.83 | 2.22 (0.97–5) | 0.054 | 5 (1.16–25) | 0.02 |
| NLR (by 3.8283) | 5.51 | 3.12 (1.61–6.25) | <0.001 | 3.03 (1.44–6.25) | 0.002 |
| Gamma delta T cells, cells/ml (by 17) | 61 | 0.52 (0.27–0.99) | 0.04 | 0.39 (0.18–0.84) | 0.014 |
| Myeloid dendritic cells, cells/ml (by 2.912) | 5.94 | 0.28 (0.13–0.56) | <0.001 | 0.40 (0.18–0.88) | 0.019 |
| Plasmacytoid dendritic cells/ml (by 2.3667) | 2.37 | 0.4 (0.16–1.0) | 0.04 | ||
| B cells, cells/ml (by 70.86) | 187.79 | 0.37 (0.18–0.75) | 0.004 | 0.42 (0.19–0.90) | 0.023 |
| B regulatory cells, cells/ml (by 3.948) | 22.7 | 0.41 (0.20–0.81) | 0.009 | 0.28 (0.13–0.62) | <0.001 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.