Abstract
Abstract 606
alloHCT is offered with curative intent to patients with hematologic malignancies, and conventionally-computed survival estimates are offered for prognosticating outcomes. However, conventionally-computed survival estimates do not take into account elapsed time (and changing hazards with time survived); conditional survival overcomes these limitations, by calculating the probability of survival after having already survived a certain period of time – such data are unavailable for alloHCT recipients. We describe cause-specific (relapse-, GvHD-, treatment-related) conditional survival after alloHCT, providing clinically relevant information for patients who have survived 6 mos, 1, 2, and 5y after alloHCT.
From 1976 to 2006, 2,427 consecutive patients received alloHCT for a hematologic malignancy at a single institution (median age: 34.7y [0.6–72.5]). Vital status and cause of death were determined using National Death Index, Social Security Death Index and medical records.
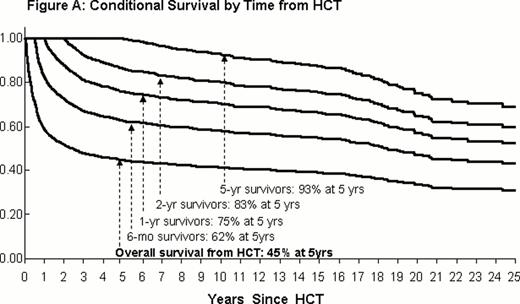
As of 12/31/2007, a total of 1413 deaths (58% of the cohort) were observed; 39% attributed to recurrent disease; 34% to GvHD; 12% to infection; 5% to cardiopulmonary disease; 2% to subsequent malignant neoplasm (SMNs); and 8% to other causes. Conventionally-computed probability of survival was 44.6% at 5y and 41.2% at 10y from alloHCT. On the other hand, conditional on survival for 6 mo, 1, 2, and 5y after alloHCT, 5-y survival rates were 62%, 75%, 83%, and 93%, respectively (Figure A). The cohort was at a 40-fold increased risk of any death compared with the general population (95%CI=38.2–42.4); at a 25.6-fold increased risk of death due to pulmonary complications, 3.3-fold risk due to SMNs, and 2.3-fold risk due to cardiovascular complications. Among patients followed for 15+y after HCT, the risk of all-cause mortality was 2.6-fold that of the general population (95%CI=1.8–3.7). Standardized mortality ratios (SMR) and cause-specific conditional mortality rates by primary diagnosis are summarized in the Table.
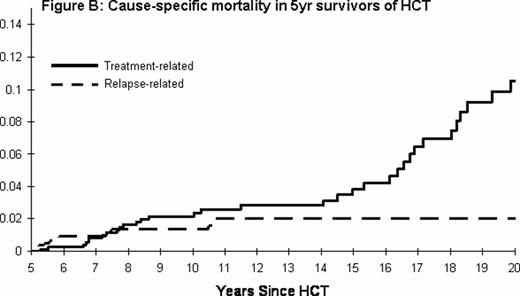
Individuals who survived the first 5y had negligible (≤5%) risk of relapse- and GvHD-related mortality over the subsequent 5y. Treatment-related mortality increased over time; among those who survived 5y, treatment-related mortality rates exceeded relapse-related mortality (Figure B). After adjustment for demographics, underlying diagnosis and treatment era, individuals with chronic GVHD (cGVHD) had a significantly lower risk of relapse-related mortality (RR=0.43, 95%CI=0.4–0.5) compared to those without cGVHD.
The projected 5-y survival rates improve conditional on time survived from alloHCT; 5-y survival exceeds 93% for those who have already survived 5y. However, alloHCT recipients who have survived 15+y continue to remain at increased risk of death compared to the general population. cGVHD is associated with decreased risk of relapse-related mortality. Both relapse-related and GvHD-related mortality rates decline with time, such that, among those who have survived 5y, treatment-related mortality exceeds relapse-related mortality. Conditional survival estimates provide clinically relevant prognostic information, helping inform preventive and interventional strategies.
Cause-specific mortality in patients undergoing allogeneic HCT
| . | . | From alloHCT . | 1 yr survivors . | 2 yr survivors . | 5 yr survivors . | ||||
|---|---|---|---|---|---|---|---|---|---|
| . | . | 5-y mortality (%) . | SMR (95%CI) . | 5-y mortality (%) . | SMR (95%CI) . | 5-y mortality (%) . | SMR (95%CI) . | 5-y mortality (%) . | SMR (95%CI) . |
| All Patients | Relapse | 18.6 | 40.3 (38.2–42.4) | 11.9 | 12.2 (11.1–13.4) | 6.5 | 7.6 (6.7–8.6) | 1.4 | 3.5 (2.9–4.3) |
| GvHD | 16.4 | 8.7 | 6.6 | 2.0 | |||||
| TRM | 11.5 | 3.3 | 5.0 | 2.1 | |||||
| ALL (n=635) | Relapse | 25.6 | 63.9 (57.7–70.0) | 18.7 | 21.1 (17.5–24.8) | 12.3 | 11.8 (9.2–14.8) | 1.8 | 4.0 (2.0–6.0) |
| GvHD | 17.3 | 10.9 | 7.1 | 0.8 | |||||
| TRM | 13.3 | 3.0 | 0.9 | 2.1 | |||||
| AML (n=749) | Relapse | 22.5 | 48.3 (43.9–52.7) | 12.8 | 14.1 (11.7–16.5) | 7.0 | 9.3 (7.4–11.4) | 1.1 | 4.6 (3.3–6.4) |
| GvHD | 12.2 | 9.0 | 6.9 | 1.5 | |||||
| TRM | 12.2 | 3.4 | 5.7 | 2.1 | |||||
| CML (n=596) | Relapse | 7.6 | 22.3 (19.7–24.9) | 4.6 | 7.4 (5.9–8.9) | 1.6 | 4.9 (3.8–6.3) | 0.7 | 2.8 (1.9–3.9) |
| GvHD | 18.9 | 7.7 | 6.9 | 2.2 | |||||
| TRM | 7.3 | 2.7 | 3.6 | 2.4 | |||||
| NHL (n=235) | Relapse | 21.4 | 45.9 (38.2–53.6) | 16.9 | 13.3 (9.1–17.6) | 12.6 | 8.6 (5.6–12.7) | 5.0 | 2.6 (0.9–5.6) |
| GvHD | 17.7 | 6.2 | 5.6 | 0 | |||||
| TRM | 11.0 | 6.4 | 3.5 | 3.3 | |||||
| MDS (n=212) | Relapse | 12.5 | 35.3 (28.8–41.8) | 7.1 | 7.5 (4.4–10.6) | 2.1 | 4.2 (2.3–7.1) | 2.0 | 3.5 (1.5–6.7) |
| GvHD | 20.5 | 8.7 | 10.7 | 9.8 | |||||
| TRM | 16.4 | 3.1 | 2.0 | 0 | |||||
| . | . | From alloHCT . | 1 yr survivors . | 2 yr survivors . | 5 yr survivors . | ||||
|---|---|---|---|---|---|---|---|---|---|
| . | . | 5-y mortality (%) . | SMR (95%CI) . | 5-y mortality (%) . | SMR (95%CI) . | 5-y mortality (%) . | SMR (95%CI) . | 5-y mortality (%) . | SMR (95%CI) . |
| All Patients | Relapse | 18.6 | 40.3 (38.2–42.4) | 11.9 | 12.2 (11.1–13.4) | 6.5 | 7.6 (6.7–8.6) | 1.4 | 3.5 (2.9–4.3) |
| GvHD | 16.4 | 8.7 | 6.6 | 2.0 | |||||
| TRM | 11.5 | 3.3 | 5.0 | 2.1 | |||||
| ALL (n=635) | Relapse | 25.6 | 63.9 (57.7–70.0) | 18.7 | 21.1 (17.5–24.8) | 12.3 | 11.8 (9.2–14.8) | 1.8 | 4.0 (2.0–6.0) |
| GvHD | 17.3 | 10.9 | 7.1 | 0.8 | |||||
| TRM | 13.3 | 3.0 | 0.9 | 2.1 | |||||
| AML (n=749) | Relapse | 22.5 | 48.3 (43.9–52.7) | 12.8 | 14.1 (11.7–16.5) | 7.0 | 9.3 (7.4–11.4) | 1.1 | 4.6 (3.3–6.4) |
| GvHD | 12.2 | 9.0 | 6.9 | 1.5 | |||||
| TRM | 12.2 | 3.4 | 5.7 | 2.1 | |||||
| CML (n=596) | Relapse | 7.6 | 22.3 (19.7–24.9) | 4.6 | 7.4 (5.9–8.9) | 1.6 | 4.9 (3.8–6.3) | 0.7 | 2.8 (1.9–3.9) |
| GvHD | 18.9 | 7.7 | 6.9 | 2.2 | |||||
| TRM | 7.3 | 2.7 | 3.6 | 2.4 | |||||
| NHL (n=235) | Relapse | 21.4 | 45.9 (38.2–53.6) | 16.9 | 13.3 (9.1–17.6) | 12.6 | 8.6 (5.6–12.7) | 5.0 | 2.6 (0.9–5.6) |
| GvHD | 17.7 | 6.2 | 5.6 | 0 | |||||
| TRM | 11.0 | 6.4 | 3.5 | 3.3 | |||||
| MDS (n=212) | Relapse | 12.5 | 35.3 (28.8–41.8) | 7.1 | 7.5 (4.4–10.6) | 2.1 | 4.2 (2.3–7.1) | 2.0 | 3.5 (1.5–6.7) |
| GvHD | 20.5 | 8.7 | 10.7 | 9.8 | |||||
| TRM | 16.4 | 3.1 | 2.0 | 0 | |||||
TRM=Treatment related mortality
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.