Abstract
Abstract  662
662
In the last 10 years IM was added to chemotherapy to improve outcome of adult patients (pts.) with Ph+ ALL, with encouraging results. The Northern Italy Leukemia Group (NILG) designed a clinical trial with chemotherapy plus short IM pulses (Bassan et al, JCO 2010; 28:3644–52) aiming to increase the CR rate, limit incidence of early failures and increase the number of patients proceeding to SCT with subsequent improvement of survival.
To analyze the long-term results in Ph+ ALL pts. treated with chemotherapy plus IM, in comparison to a prior cohort treated without IM.
IM 600 mg/d was given orally for 7 consecutive dd. with each chemotherapy block, starting from day 15 of induction (IDR/VCR/PDN±ASP) and day –3 of consolidation courses (5x IDR/VCR/CY/DEXA; 2x HD-MTX/ARA-C). All pts. received CNS chemo-radioprophylaxis and were eligible to allogeneic SCT, or alternatively to HD therapy with autologous SCT and long-term maintenance with 6MP/MTX and intermittent IM.
Between April '00 and November '08, 100 out of 404 pts. enrolled into NILG trial 09/00 had Ph+ ALL (median age 46 years, range 19–66; male 54). The pts. belonged to two subsequent treatment groups: control arm (IM-, n=35) and IM+ arm (n=65), of whom 59 received IM during induction/consolidation and 6 during consolidation only (pts. included in IM- cohort for remission induction analysis and in IM+ cohort afterwards). From March 2005 ASP was omitted during induction due to increased toxicity, so that in the IM+ group 20 pts. received ASP and 39 did not.
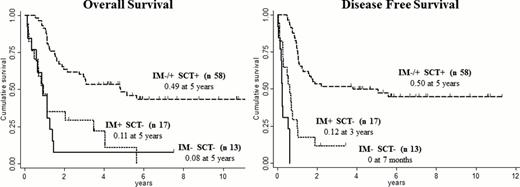
The complete remission (CR) rate was: 33/41 (80.5%) in IM- vs. 55/59 (93%) in IM+ pts. (p=0.05). With regard to the use of ASP in IM+ group, CR rate was: 16/20 (80%) with ASP vs. 39/39 (100%) without ASP (p=0.004). With a median follow-up of 1,6 years (maximum 11.3), 24/60 (40%) IM+ pts. are alive in 1st CR compared to 5/28 (18%) IM- pts., (p=0.04). Estimated 5-year OS, DFS and early relapse rates were significantly improved and reduced (relapse risk within 6 mos.), respectively, in IM+ vs. IM- group: OS 0.38 vs. 0.23 (p=0.012), DFS 0.40 vs. 0.25 (p=0.015) and relapse risk 0.05 vs. 0.24 (p=0.003). The probability to receive a SCT (autologous or allogeneic) was increased in IM+ pts. (72% vs. 54%), a difference that was statistically significant for allogeneic SCT (63% vs. 39%, p=0.04). In a cumulative analysis, patients receiving a SCT had the best outcome regardless of prior IM use (n=58; 5-years OS 0.49 and DFS 0.50), while in pts. unable to reach SCT outcome was slightly better in those exposed to IM (Figure). Forty CR pts. (28 IM+ and 12 IM-), were evaluable for minimal residual disease (MRD) response at weeks 10–22. PCR-negativity at weeks 10 and 16 was tendentially higher in IM+ group (32% and 37,5%) rather than IM- pts. (25% and 12,5%, p=ns).
This long-term update confirms that short IM pulses in combination with chemotherapy increased the rate of CR, reduced incidence of early failures, and allowed to increase the feasibility of SCT, with a marked outcome improvement. An allogeneic SCT appears the best consolidation option for Ph+ ALL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract