Abstract
Abstract  691
691
Tyrosine kinase inhibitor (TKI) therapy has become the standard treatment for patients with chronic phase chronic myelogenous leukemia (CML-CP). Compared with imatinib, dasatinib is known to induce a faster and better response as a first- and second-line treatment. A unique effect of dasatinib treatment is the induction of clonal lymphocytosis with large granular lymphocyte (LGL) morphology, presumed to be the effect of off-target kinase inhibition. These LGLs are known to possess either cytotoxic T-cell (CTL) or natural-killer (NK) cell phenotype. Several reports have shown that this clonal LGL expansion is associated with a better response to dasatinib treatment.
Purpose: To prospectively analyze the immunoprofile of Japanese patients treated with dasatinib, and to correlate the increase of lymphocytes and their subsets (LGL, CTL and NK cells) with the clinical efficacy of dasatinib.
Japanese patients with CML-CP who were resistant or intolerant to first-line imatinib therapy participated in the prospective phase II study assessing the efficacy and safety of dasatinib. Peripheral blood LGL, CTL and NK cell counts before and 2 weeks, 1 month (M), 3M, and 6M after the initiation of treatment were analyzed at the central laboratory (BML Inc.) by flow cytometry. LGL, CTL and NK cells were defined as CD57+/CD14-, CD8+/CD4- and CD56+/CD3- cells, respectively. Lymphocytosis was defined as a lymphocyte count of >3.0×109/L. The clinical efficacy of dasatinib was evaluated at 12M as complete molecular response (CMR) or less than CMR by peripheral blood quantitative RT-PCR (BML Inc.). The full data set was available for 50 out of 65 patients and was included in this analysis.
The median age of the patients enrolled was 57 years (range: 16 – 87 years). There were 37 male and 13 female patients. Twenty patients were switched to dasatinib due to intolerance to imatinib and 30 due to resistance. Lymphocytosis was observed in 19 patients (38%) at 3M. Of those 19 patients, 14 (73.7%) had lymphocytosis persisting at 6M. In total, 21 patients (42%) achieved CMR at 12M.
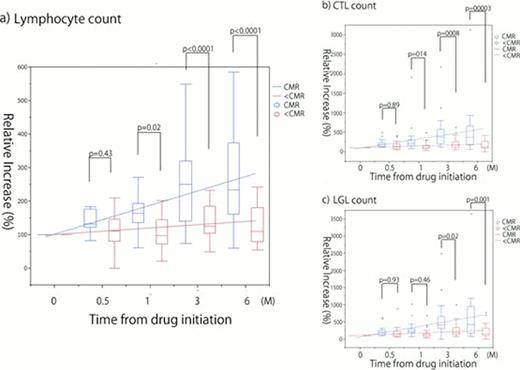
The absolute count of lymphocytes, LGL, CTL or NK cells, did not differ significantly between patients who achieved CMR at 12M and those who did not (p>0.05). However, there were significant differences between these two groups in the relative increase of these cell counts. Relative increase of lymphocytes compared to baseline as early as 2 weeks after initiation of treatment was identified by univariate analysis as a significant factor associated with CMR at 12M (p=0.0348). This increase persisted at each time point observed until 6M. As for the different subsets of lymphocytes, the relative increase of CTL at 3 and 6M and LGL at 1, 3 and 6M were also significantly associated with a higher rate of CMR at 12M. When adjusted for possible confounding factors (age, sex, performance status, whether 1st or 2nd CP, resistance or intolerance to imatinib), the relative increase of lymphocytes at 1, 3 and 6M, CTL and LGL at 3 and 6M remained significant (Fig a-c).
Patients who showed an increase of lymphocytes of over 1.5-fold at 1M showed a significantly higher rate of CMR at 12M (66.7% vs 25.8%, p=0.0007). Similar differences were seen in patients with increases of over 2-fold in CTL, LGL and NK cells (70.6% vs 22.6%, p=0.0011; 74% vs 21%, p=0.0003; and 57.9% vs 28.6%, p=0.0444). Detailed analysis at 3M showed a further significant difference in the treatment effect. An increase of over 2-fold in lymphocytes (81.3% vs 21.2%, p<0.0001), and of over 5-fold in CTL (85.7% vs 30%, p<0.0001), LGL (66.7% vs 30.3%, p=0.0001) and NK cells (75% vs 31.6%, p<0.0001) compared to baseline was associated with a significantly increased probability of CMR at 12M.
Lymphocytosis after the initiation of dasatinib was seen in a substantial proportion of Japanese patients treated with dasatinib. A relative increase of lymphocytes together with LGL, CTL and NK cells, uniformly defined by flow cytometry, at 1 and 3M after the initiation of treatment were associated with a higher rate of CMR at 12M. To our knowledge, this is the first large prospective study analyzing the clinical significance of lymphocytosis associated with dasatinib therapy in Japanese patients with CML-CP using flow cytometry. Our results suggest that a relative increase of lymphocytes as early as 1M after the initiation of dasatinib is a reliable predictive marker for achieving CMR at 12M.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract