Abstract
Abstract 935
Lytic bone disease is a frequent complication of multiple myeloma (MM). Biochemical markers of bone metabolism provide information on bone dynamics and reflect activity in the bones. Several studies show that different bone markers are altered in myeloma patients, reflect the extent of bone disease and correlate with survival in the conventional chemotherapy era. Nevertheless, there is almost no information about their impact on the survival of myeloma patients who are treated upfront with novel agents.
To address this issue we studied 122 consecutive, unselected, newly diagnosed patients with symptomatic MM (66M/56F, median age 71 years, range 36–88 years) who were diagnosed and treated in a single center (University of Athens, Greece). All patients received upfront novel agents: 75 patients IMiDs-based and 47 patients bortezomib-based regimens. The following bone remodeling markers were evaluated in the patients' serum before the administration of any kind of therapy: i) osteoclast regulators: sRANKL and osteoprotegerin (OPG); ii) osteoblast inhibitor dickkopf-1 (Dkk-1); iii) bone resorption markers: CTX and TRACP-5b; and iv) bone formation markers: bone-specific alkaline phosphatase (bALP) and osteocalcin. The above molecules were also measured in 36 gender- and age-matched, healthy controls. Evidence of bone involvement was documented using plain radiographs and MRI of the spine in all patients.
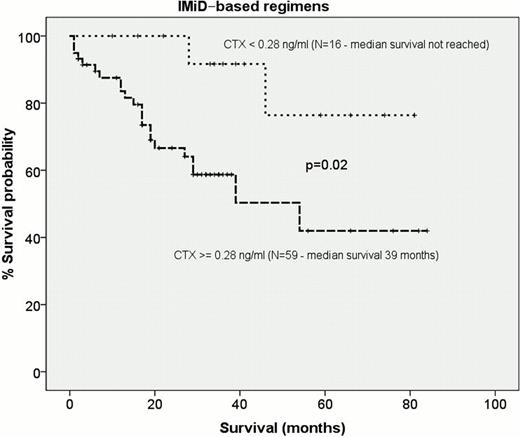
Twenty-five (20%) patients had ISS-I disease, while 46 (37%) patients had ISS-II and 51 (41%) stage ISS-III disease. Fifty-eight (47%) patients had Hb<10 g/dl and 24 (19%) patients had serum creatinine >2 mg/dl. The presence of lytic bone disease was documented in 76% of the patients. MRI evaluation of the spine revealed that 41% of the patients had focal, 38% diffuse, 19% normal, and 2% a variegated pattern of marrow involvement. At diagnosis, MM patients had increased serum concentrations of sRANKL (mean±SD: 0.4±0.5 pmol/L vs. 0.1±0.2 pmol/L; p<0.001), OPG (6.4±3.3 pmol/L vs. 4.2±1.7 pmol/L; p<0.001), CTX (0.90±0.97 ng/ml vs. 0.3±0.2 ng/ml; p<0.001),TRACP-5b (2.7±2 U/L vs. 1.6±0.7 U/L; p<0.001), Dkk-1 (59.4±38.7 ng/ml vs. 32.8±13 ng/ml; p<0.001) and sRANKL/OPG ratio (0.08±0.13 vs. 0.04±0.05; p=0.003) and decreased levels of bALP (21.6±15.1 U/L vs. 29.4±7.8 U/L; p=0.003) compared to controls, while their levels correlated with the extend of bone disease. Patients with diffuse pattern had higher CTX concentrations compared to all other others (0.95±1.2 ng/ml vs. 0.6±0.51 ng/ml; p=0.04). The median survival of all patients was 59 months. In the univariate analysis, among the studied bone markers, only CTX, as a continuous variable, was predictive of survival (HR: 1.292, p=0.024). Patients with low CTX concentrations (<0.28 ng/ml; lower quartile; N=29) had superior survival compared to patients with higher CTX concentrations (not reached vs. 54 months respectively; p=0.034). This was more profound in patients treated with IMiDs-based regimens: the median survival of those with low CTX levels (<0.28 ng/ml) has not been reached yet vs. 39 months of all others (p=0.02; Figure). There was no difference regarding the effect of CTX on survival between patients who received upfront thalidomide- or lenalidomide-based regimens. On the contrary, in patients who were treated with bortezomib-based schemes, high CTX could not define a poor prognosis group of patients. In patients with normal or focal MRI pattern of bone marrow involvement, low CTX concentrations also correlated with superior survival compared to all other patients (not reached vs. 54 months respectively; p=0.04). Serum LDH (as dichotomous variable >225 U/L; p=0.011, and as continuous variable; p=0.019), ISS stage (p=0.02) and anemia (Hb<10 g/dl; p=0.01) were also associated with survival in the univariate analysis. The presence of osteolytic disease at diagnosis had no impact on survival. In the multivariate analysis only ISS (p=0.02) and LDH (>225 U/L; p=0.038) were predictive for survival.
Our study suggests that in the era of novel agents, only CTX, among 7 serum bone remodeling markers, correlated with survival. In particular, high CTX levels can distinguish a subset of patients who receive frontline IMiDs-based therapies and who have poor prognosis. This was not observed with bortezomib-based therapies, possibly due to the beneficial effect of bortezomib on bone metabolism.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.