In this issue of Blood, Iland et al report that the addition of arsenic trioxide during induction and consolidation can substantially reduce the amount of chemotherapy and the duration of consolidation to achieve excellent outcomes in patients with newly diagnosed acute promyelocytic leukemia (APL; see figure).1
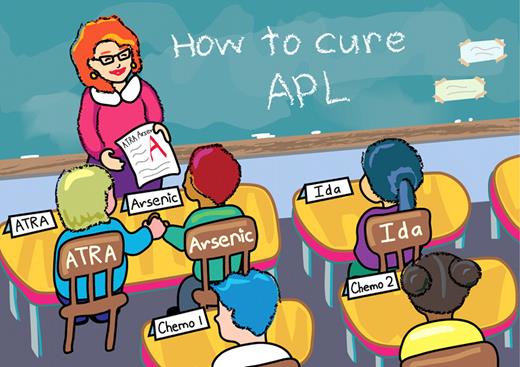
The combination of ATRA and arsenic with varying amounts of chemotherapy has been studied in newly diagnosed APL patients. Iland et al report one of the best outcomes observed in APL studies using ATRA plus arsenic during induction and consolidation with 4 doses of idarubicin in induction only. Professional illustration by Noel Sirivansanti/Xavier Studio.
The combination of ATRA and arsenic with varying amounts of chemotherapy has been studied in newly diagnosed APL patients. Iland et al report one of the best outcomes observed in APL studies using ATRA plus arsenic during induction and consolidation with 4 doses of idarubicin in induction only. Professional illustration by Noel Sirivansanti/Xavier Studio.
The therapeutic benefit of arsenic was first recognized more than 2400 years ago by Greek and Chinese healers who used arsenic to treat a variety of diseases. However, as medicine evolved in the 20th century, the enthusiasm for arsenic waned rapidly, and its reputation as a poison and an environmental toxin further discouraged its use. Then, in the early 1970s, a group of investigators from Harbin Medical University in China used a crude solution of arsenic trioxide (As2O3) and observed complete remissions (CRs) in two-thirds of the patients with relapsed APL.2 A series of clinical trials quickly followed and confirmed the striking and specific activity of As2O3 in APL.3
In the frontline setting, As2O3 alone induced CR in approximately 80% of patients, but long-term follow-up studies reported a relapse rate exceeding 20% in high-risk patients.4,5 When As2O3 was combined with standard chemotherapy-based consolidation, fewer relapses occurred across all risk groups despite less cumulative doses of anthracyclines and cytarabine.6,7 In an attempt to further reduce chemotherapy-associated toxicities and to build on synergism between all-trans retinoic acid (ATRA) and As2O3, subsequent clinical trials combined ATRA and As2O3 with minimal chemotherapy, and observed an outcome comparable to that reported with ATRA plus anthracycline-based chemotherapy.8,9
Here, Iland and colleagues report the outcome of 124 newly diagnosed APL patients treated with ATRA and As2O3 both during induction and consolidation with limited chemotherapy exposure.1 In the study, patients with de novo APL received induction consisting of ATRA, intravenous As2O3, and 4 doses of age-adjusted idarubicin (maximum cumulative dose = 48 mg/m2). All patients regardless of presenting white blood cell (WBC) counts received prednisone as prophylaxis for APL differentiation syndrome. CR was achieved in 95% of patients with an early death rate of 3.2% (defined as death during induction). Notably, the trial included only 2 consolidation cycles consisting of ATRA and intravenous As2O3, administered on continuous schedule during consolidation 1 and 5 d/wk during consolidation 2. All patients achieved molecular CR by the end of consolidation, and all received maintenance therapy for 2 years consisting of intermittent ATRA, oral methotrexate, and 6-MP. Two of the 112 patients who completed consolidation and maintenance therapy relapsed, with an impressive 98% disease-free survival rate at 2 years. Sanz risk stratification and FLT3 mutational status did not affect these outcomes. Importantly, this treatment approach appeared feasible with more than 90% of patients receiving at least 80% of the maximum total dose of intravenous As2O3 during both consolidation cycles.
While longer follow-up will be required to confirm the durability of remission and to monitor long-term toxicities of As2O3-based therapy, the excellent outcome reported by Iland and colleagues challenges the role of cytarabine in the frontline APL therapy even in high-risk patients, and, along with work by Ravandi et al,9 suggests that the majority of APL patients may be cured with little or no chemotherapy. However, several questions remain unanswered. First, the optimal number of consolidation cycles with As2O3-containing frontline therapy has not been addressed adequately. Investigators at the MD Anderson Cancer Center incorporated 4 consolidation cycles into their frontline regimen consisting of ATRA plus As2O3 with or without gemtuzumab.9 Iland et al in this article used a very similar regimen, but included only 2 cycles of consolidation and added idarubicin during induction. Despite the considerably shorter consolidation compared with other studies, Iland and colleagues observed the remarkable outcome, which is a testament to the potency of ATRA and As2O3 combination and suggests that shorter consolidation may be sufficient when idarubicin is added during induction.1 Second, the optimal schedule of intravenous As2O3 during consolidation is unknown. Continuous, 6 d/wk and 5 d/wk schedules have all been used, but have never been compared with one another. The dose-dependent As2O3-associated toxicity noted by Iland et al favors the 5 d/wk schedule, which may be particularly suitable for older patients. Third, the role of maintenance with the As2O3-based therapy remains controversial. All of the patients in this study achieved molecular CR after consolidation.1 Given recent studies suggesting that maintenance may not be required for patients in molecular CR after standard ATRA plus anthracycline-based chemotherapy,7,10 future trials of As2O3-based frontline therapy need to carefully examine the role of maintenance. Lastly, it is unclear whether additional cytotoxic agents are required for non–high-risk patients treated with ATRA plus As2O3-based therapy. The MD Anderson study reported that non–high-risk patients without hyperleukocytosis during induction remained free of relapse without any chemotherapy exposure.9 Iland et al used idarubicin in all patients regardless of the presenting WBC counts,1 and it is difficult to glean from the study whether idarubicin is responsible for the excellent outcome or can be safely omitted in non–high-risk patients. Future trials incorporating risk-adapted anthracycline administration during induction will hopefully be able to answer this question.
The work by Iland et al highlights the remarkable ability of the ATRA and As2O3 combination to treat APL with minimal anthracyclines, and paves the way to cure the disease only with the rationally combined targeted agents. However, the challenge remains to define appropriate chemotherapy exposure during induction, determine the role of oral As2O3, evaluate the optimal number of consolidation cycles, and examine the requirement for maintenance with As2O3-based frontline therapy.
Conflict-of-interest disclosure: The author declares no competing financial interest. ■