Abstract
miR-155 acts as an oncogenic miR in B-cell lymphoproliferative disorders, including Waldenstrom macroglobulinemia (WM) and chronic lymphocytic leukemia, and is therefore a potential target for therapeutic intervention. However, efficient targeting of miRs in tumor cells in vivo remains a significant challenge for the development of miR-155–based therapeutics for the treatment of B-cell malignancies. In the present study, we show that an 8-mer locked nucleic acid anti–miR-155 oligonucleotide targeting the seed region of miR-155 inhibits WM and chronic lymphocytic leukemia cell proliferation in vitro. Moreover, anti–miR-155 delivered systemically showed uptake in the BM CD19+ cells of WM-engrafted mice, resulting in the up-regulation of several miR-155 target mRNAs in these cells, and decreased tumor growth significantly in vivo. We also found miR-155 levels to be elevated in stromal cells from WM patients compared with control samples. Interestingly, stromal cells from miR-155–knockout mice led to significant inhibition of WM tumor growth, indicating that miR-155 may also contribute to WM proliferation through BM microenvironmental cells. The results of the present study highlight the therapeutic potential of anti–miR-155–mediated inhibition of miR-155 in the treatment of WM.
Introduction
miRs are a class of small, noncoding RNAs (18-23 nt) that control gene expression at the posttranscriptional level by repressing translation or by promoting degradation of the target mRNAs.1–3 miRs play essential roles in many biologic processes, including development of the immune system and immune response.4,5 Moreover, deregulated expression of specific miRs is associated with a wide variety of diseases, including both solid and hematopoietic malignancies.6,7
Waldenström macroglobulinemia (WM) is a low-grade lymphoproliferative disorder characterized by the presence of an IgM monoclonal protein in the blood and monoclonal small lymphocytes and lymphoplasmacytoid cells in the BM.8 In chronic lymphocytic leukemia (CLL), a combination of predominant resistance to apoptosis and continuing proliferation leads to progressive accumulation of phenotypically mature malignant lymphocytes.9 Both diseases are incurable, low-grade, non-Hodgkin B-cell lymphomas.
Epigenetics, including DNA methylation, chromatin remodeling, and miR-mediated regulation of gene expression, has been implicated recently in the pathogenesis of B-cell malignancies.10,11 We and others have demonstrated that primary WM and CLL cells present with increased expression of miR-155.12,13 Furthermore, overexpression of miR-155 in B cells of transgenic mice leads to polyclonal pre-B cell proliferation, followed by lymphoblastic leukemia/high-grade lymphoma, indicating that miR-155 plays a crucial role in the pathogenesis of B-cell malignancies and is therefore a potential target for therapeutic intervention. However, reports on pharmacologic inhibition of miR-155 in mouse models of B-cell lymphoma have been lacking.
Locked nucleic acid (LNA) is a conformational analog of RNA in which the ribofuranose ring in the sugar-phosphate backbone is locked in an RNA-like, C3′-endo conformation.14 This results in high binding affinity between single-stranded, LNA-modified anti-miR oligonucleotides and their complementary miR targets. Several studies have reported on the inhibition of miR function using high-affinity 15- to 16-nt LNA-modified DNA phosphorothioate oligonucleotides targeting the 5′ region of the mature miR.15–21 Furthermore, a recent study described a method for antagonizing miR function using 8-mer LNA oligonucleotides complementary to the miR seed region, which were called “tiny LNAs.”22
In the present study, we assessed the efficacy of an 8-mer seed-targeting anti–miR-155 in inhibiting miR-155 function in low-grade non-Hodgkin B-cell lymphoma cells in vitro and in a mouse xenograft model of WM in vivo.
Methods
Cells and reagents
Primary WM cells were collected from the BM of WM patients using CD19+ microbead selection (Miltenyi Biotec) with more than 90% purity, as confirmed by flow cytometric analysis with an mAb against human CD19 (BD Biosciences).13 Similarly, CD19+ cells were isolated from the BM and peripheral blood of 3 healthy donors and used as controls. Approval for these studies was obtained from the Dana-Farber Cancer Institute Institutional Review Board. Informed consent was obtained from all patients and healthy volunteers in accordance with the Declaration of Helsinki protocol. BCWM1, MEC1, and HEK293 cell lines were used in this study. BCWM.1 is a previously described WM cell line derived from CD19+-selected BM lymphoplasmacytic cells isolated from a patient with untreated WM,23 MEC1 is a cell line derived from B-chronic lymphocytic leukemia in prolymphocytoid transformation,24 and HEK293 is a human embryonic kidney epithelial cell line (CRL-1573; ATCC). The cell lines were cultured as described previously.13 BCWM1, MEC1, and mCherry-Luc+-BCWM1 cells were cultured at 37°C in RPMI 1640 medium containing 10% FBS (Sigma-Aldrich), 2mM l-glutamine, 100 U/mL of penicillin, and 100 μg/mL of streptomycin (Invitrogen). mCherry-Luc+-BCWM1 cells were generated using lentiviral infection and were a gift from Dr Andrew Kung (Dana-Farber Cancer Institute). Human stromal cells negatively selected by CD19+ microbeads from normal healthy donors or WM patients were cultured at 37°C in DMEM containing 20% FBS, 2mM l-glutamine, 100 U/mL of penicillin, and 100 μg/mL of streptomycin. Mice stromal cells were isolated and cultured as a reference.25 HEK293 cells stably expressing copepod green fluorescent protein (copGFP) control plasmid or stably expressing pre–miR-155 were generated using PMIRH155PA-1 or pCDH-CMV-MCS-EF1-copGFP cDNA Cloning and Expression Vector (System Biosciences) by lentiviral infection and sorting using the GFP marker. HEK293 and mice stromal cells were cultured at 37°C in DMEM containing 20% FBS, 2mM l-glutamine, 100 U/mL of penicillin, and 100 μg/mL of streptomycin.
DNA synthesis and cytotoxicity assay
GEP
Total RNA from BCWM1 cells treated with anti–miR-155 or LNA scramble control oligonucleotide, respectively, for 48 hours were isolated using the RNeasy kit (QIAGEN) following the manufacturer's instructions and hybridized on an Affymetrix U133A 2.0 array chip. Gene-expression profiling (GEP) data were analyzed using dChip 2010.01 software (http://biosun1.harvard.edu/complab/dchip/). Candidate target mRNAs for miR-155 were identified using the algorithms TargetScan (http://genes.mit.edu/targetscan/), PicTar (http://pictar.bio.nyu.edu/), and RNAhybrid (http://bibiserv.techfak.uni-bielefeld.de/rnahybrid/). All microarray data are available on the Gene Expression Omnibus public database under accession no. GSE39189.
qRT-PCR
Total RNA of cells was isolated with RNeasy kit (QIAGEN). cDNA was synthesized using SuperScript cDNA synthesis kit (Invitrogen) and quantitative RT-PCR (qRT-PCR) reactions were performed using SYBR Master Mix (SA Bioscience) with designated primers relative to 18S expression by StepOnePlus Real-Time PCR System (Applied Biosystems) in triplicate. TaqMan microRNA Assay kits (Applied Biosystem) were used for quantifying hsa-miR-155 levels relative to RNU6B expression.
Luciferase assays
The oligonucleotides comprising the wild-type or mutated miR-155 target sequences were synthesized by Integrated DNA Technologies, and annealed to be cloned into pMiRGLO vector (Promega) for luciferase reporter assays. The miR-155 target sequences within the 3′-untranslated regions (3′-UTRs) of each target mRNA were predicted by TargetScan, and the sequences are shown below with the wild-type and mutated miR-155 seed match sites underlined. Each construct was confirmed by sequencing at the Molecular Biology Core Facility of Dana-Farber Cancer Institute.
MAFB wild-type: 5′ AAAUACAAAAAAUCUGCAUUAAA 3′ (position 628-634); MAFB mutated: 5′ AAAUACAAAAAAUCUCGUAAUAA 3′; SH3PXD2A wild-type: 5′ GGAAAUUUCACACUGGCAUUAAC 3′ (position 5426-5432); SH3PXD2A mutated: 5′ GGAAAUUAGUGACUGCGUAAUAC 3′; SHANK2-1 wild-type: 5′ GUUAUUGAACAAGCAAGCAUUAU 3′ (position 3148-3154); SHANK2-1 mutated: 5′ GUUAUUGAACAAGCAUCGUAAUU 3′; SHANK2-2 wild-type: 5′ AUCAUGAGAUGAAUGAGCAUUAC 3′ (position 2190-2196); and SHANK2-2 mutated: 5′ AUCAUGAGAUGAAUGUCGUAAUC 3′.
HEK293 cells were seeded into 96-well plates and transfected with the constructs harboring wild-type or mutated 3′-UTR target sequences or empty vector as a control. Luciferase activity was measured using the Dual-Glo Luciferase Assay System (Promega). Renilla luciferase activity was normalized to corresponding firefly luciferase activity and is shown as a relative percentage of the control. Experiments were done in triplicate and repeated 3 times.
In vivo studies
Approval of animal studies was obtained by the Dana-Farber Cancer Institute Institutional Animal Care and Use Committees. Six- to 8-week-old, female SCID or Balb/c mice were obtained from Charles River Laboratories. Anesthesia was performed by IP injections of ketamine (80 mg/kg body weight; Bedford Laboratories)/xylazine (12 mg/kg body weight; Lloyd Laboratories).
Balb/c mice were treated with a single IV tail-vein injection of fluorescein amidite (FAM)–labeled anti–miR-155 (synthesized with a complete phosphorothioate backbone and fully LNA modified22 ) or with saline as a control. Live in vivo confocal imaging was used to detect the distribution of the FAM-labeled anti-miR in the mouse BM 1 or 2 weeks after injection (Zeiss 710). Cells from mouse tissues were analyzed by immunofluorescence (Zeiss 710) and flow cytometry (BD FACSCanto II HTS).
Immediately after tail-vein injection of mCherry-Luc+-BCWM1 cells (3 × 106/mouse) in SCID mice, the mice (6 mice/group) were treated with a single IV tail-vein injection of 25 mg/kg with either anti–miR-155 or LNA scramble control, followed by weekly maintenance doses of 5 mg/kg of anti–miR-155 or LNA scramble control until the mice were killed. Mice were injected with 75 mg/kg of luciferin (Caliper Life Sciences), followed by whole-body real-time bioluminescence imaging (Xenogen IVIS imaging system; Caliper Life Sciences) performed at days 0, 14, and 19. Mice were killed by inhalation of CO2. RNA was extracted from CD19+ cells isolated from one mouse femur using CD19+ microbead selection. The other femur and the liver and spleen were fixed in formaldehyde. Tissue sections were stained as described previously13 using Abs against MAFB (Abcam) or CEBPβ (Abcam).
Statistical analysis
Data were analyzed using unpaired Student t tests comparing 2 conditions or a 1-way ANOVA with Bonferroni or Newman-Keuls correction for multiple comparisons. P < .05 was considered significant and tests were performed 2-sided. Data are presented as means and error bars in the figures depict SD.
Results
Inhibition of miR-155 decreases WM and CLL proliferation in vitro
We first examined the level of miR-155 in primary WM and CLL primary cells, as well as in IgM-secreting low-grade lymphoma cell lines (BCWM1 and MEC1) by qRT-PCR. Our data showed that miR-155 was significantly higher in these samples compared with normal donor CD19+ cells isolated from healthy subjects (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article), suggesting that miR-155 may represent a viable therapeutic target in these diseases. To inhibit miR-155 function in malignant cells, we used a fully LNA-modified 8-mer seed-targeting anti–miR-155 (supplemental Figure 2).22 To assess the uptake of anti–miR-155 into BCWM1 or MEC1 cells, we used a 5′ FAM-labeled anti–miR-155 and added the anti-miR directly to the cell suspension without any transfection reagent. The uptake of FAM-labeled anti–miR-155 into BCWM1 cells was higher than 90% as judged by flow cytometry (data not shown), which indicates efficient delivery of the 8-mer anti-miR into tumor cells. To further examine the functional effect of anti–miR-155 on BCWM1 or MEC1, we measured cell survival and cell proliferation by MTT and [H]3 thymidine uptake assays, respectively. Treatment of BCWM1 or MEC1 cells with 20μM anti–miR-155 or scramble control showed significant reduction in cell proliferation 48 hours after treatment (Figure 1A) with no change in cell cytotoxicity (data not shown), which is consistent with previous findings that miR-155 inhibition regulates cell proliferation but not cell apoptosis.13
Identification of novel miR-155 target mRNAs in WM. (A) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours. miR-155 inhibition decreases BCWM1 and MEC1 cell proliferation in vitro as evaluated by the [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (B) BCWM1 cells were treated with anti–miR-155 or scramble control for 48 hours. All of the BCWM1 cell samples were cultured and processed in parallel for total RNA extraction and GEP using Affymetrix GeneChip. Validated targets of miR-155 are shown in a heat map on the left and predicted targets of miR-155 are listed on the right. (C) qRT-PCR analysis of selected miR-155 targets in BCWM1 cells treated with anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (D) Stable HEK293 cell lines overexpressing pre-miR-155 or empty vector as a control were generated by lentiviral infection. Cells were transiently transfected with the reporter plasmid pmirGLO driving luciferase expression with a target gene fragment containing the predicted miR-155 binding site or a mutated binding site as a control. Relative luciferase activity was decreased in miR-155–overexpressing HEK293 cells transfected with plasmids harboring miR-155 target sequences compared with plasmids harboring mutated target sequences. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (E) mRNA levels of miR-155 target genes were detected by qRT-PCR from normal donor blood CD19+ cells, BCWM1 and MEC1 cells, primary WM CD19+ cells, and primary CLL cells. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. (F) mRNA levels of miR-155 target genes were detected by qRT-PCR from primary WM CD19+ cells treated with 20μM anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. (G) mRNA levels of miR-155 target genes were detected by qRT-PCR from primary CLL cells treated with 20μM anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD.
Identification of novel miR-155 target mRNAs in WM. (A) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours. miR-155 inhibition decreases BCWM1 and MEC1 cell proliferation in vitro as evaluated by the [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (B) BCWM1 cells were treated with anti–miR-155 or scramble control for 48 hours. All of the BCWM1 cell samples were cultured and processed in parallel for total RNA extraction and GEP using Affymetrix GeneChip. Validated targets of miR-155 are shown in a heat map on the left and predicted targets of miR-155 are listed on the right. (C) qRT-PCR analysis of selected miR-155 targets in BCWM1 cells treated with anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (D) Stable HEK293 cell lines overexpressing pre-miR-155 or empty vector as a control were generated by lentiviral infection. Cells were transiently transfected with the reporter plasmid pmirGLO driving luciferase expression with a target gene fragment containing the predicted miR-155 binding site or a mutated binding site as a control. Relative luciferase activity was decreased in miR-155–overexpressing HEK293 cells transfected with plasmids harboring miR-155 target sequences compared with plasmids harboring mutated target sequences. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (E) mRNA levels of miR-155 target genes were detected by qRT-PCR from normal donor blood CD19+ cells, BCWM1 and MEC1 cells, primary WM CD19+ cells, and primary CLL cells. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. (F) mRNA levels of miR-155 target genes were detected by qRT-PCR from primary WM CD19+ cells treated with 20μM anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. (G) mRNA levels of miR-155 target genes were detected by qRT-PCR from primary CLL cells treated with 20μM anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD.
Identification of novel miR-155 targets in B-cell lymphoma cells
To identify new direct miR-155 targets in B-cell lymphomas, we performed GEP on BCWM.1 cells after treatment with anti–miR-155 or scramble control for 24 or 48 hours. Based on GEP data, we found that several validated miR-155 target mRNAs, such as CEBPβ, SMAD5, and SOCS1, were up-regulated in the BCWM1 cells after treatment with anti–miR-155 compared with cells treated with scramble control (Figure 1B). Moreover, we identified 3 potential new targets of miR-155, MAFB, SHANK2, and SH3PXD2A, as predicted by TargetScan software, which were derepressed 48 hours after anti–miR-155 treatment (Figure 1B). These findings were further validated by qRT-PCR, which confirmed the array data from anti–miR-155–treated BCWM1 cells (Figure 1C).
To functionally validate the miR-155 target mRNA interactions, we generated luciferase 3′-UTR reporters for MAFB, SHANK2, and SH3PXD2A. We used an RNA hybrid to depict the miR-155 target sites in the 3′-UTRs of MAFB, SHANK2, and SH3PXD2A, followed by cloning of the wild-type and mutated target sequences into the pMiRGLO vector (supplemental Figure 3). After transfection of the luciferase reporters into HEK293 cells stably expressing copGFP control plasmid or HEK293 cells stably expressing pre-miR-155 (supplemental Figure 4), dual luciferase activity was measured. A significant repression of the luciferase activity was observed for all 3′-UTR reporters containing a perfect match target site, whereas there was no change in luciferase activity for the reporters harboring mutations in the miR-155 target site sequences, implying that MAFB, SHANK2, and SH3PXD2A are indeed bona fide targets of miR-155 (Figure 1D).
We next used qRT-PCR to determine the mRNA levels of the 6 miR-155 target genes, SMAD5, SOCS1, CEBPβ, MAFB, SHANK2, and SH3PXD2A, in BCWM1 cells from primary WM CD19+ cells, primary CLL cells, normal donor blood CD19+ cells, and BCWM1 and MEC1 cells. We found that all 6 targets were significantly down-regulated in malignant cells in WM or CLL compared with normal control CD19+ cells (Figure 1E). Moreover, treatment of primary WM CD19+ cells or primary CLL cells with 20μM anti–miR-155 for 48 hours showed a significant increase in the mRNA levels of the 6 miR-155 targets compared with scramble control–treated cells as judged by qRT-PCR (Figure 1F-G). In summary, our data indicate that SMAD5, SOCS1, CEBPβ, MAFB, SHANK2, and SH3PXD2A are negatively regulated by miR-155 in WM and CLL.
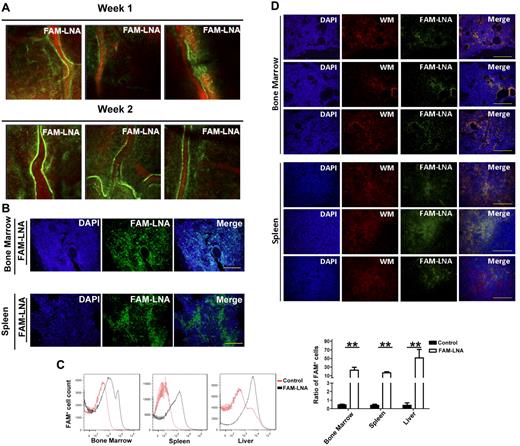
Delivery of anti–miR-155 into engrafted WM cells in recipient mice
We next investigated whether the anti–miR-155 could be delivered to the BM, where low-grade B-cell malignancies primarily reside. Balb/c mice were dosed with a single IV tail-vein injection of 25 mg/kg of FAM-labeled anti–miR-155 or saline control and examined for distribution after 1 week and 2 weeks by live in vivo confocal imaging. As shown in Figure 2A, the FAM-labeled anti–miR-155 was successfully taken up by cells present in the BM and was detected up to 2 weeks after a single tail-vein injection of the anti–miR-155 compound. We also examined the distribution of FAM-labeled anti–miR-155 in cells of other tissues in the hematopoietic system of the mice, including spleens and femoral BM, by immunofluorescence. Our data showed that the FAM-labeled anti–miR-155 was widely distributed in both the spleen and BM, which show high levels of infiltrated malignant B cells in WM and CLL (Figure 2B). Furthermore, we examined the distribution of FAM-labeled anti–miR-155 in cells from the femur, spleen, and liver using flow cytometric analysis to quantify the ratio of cells that were positive for FAM-labeled anti–miR-155. As shown in Figure 2C, there was a significant shift in the number of FAM+ cells. These data indicate that the anti–miR-155 could be efficiently delivered and taken up by cells of the hematopoietic system.
Distribution of FAM-labeled anti–miR-155 in mice. Balb/c mice were dosed with a single tail-vein injection of 25 mg/kg of FAM-labeled anti–miR-155 or saline. (A) Distribution of FAM-labeled anti–miR-155 in cells from mice calvarium BM shown by live in vivo confocal microscopy imaging. Blood vessels are shown by Evans blue staining in red and FAM-labeled anti–miR-155 in green. (B) Distribution of FAM-labeled anti–miR-155 in cells from mice organs shown by immunofluorescent imaging. Cell nuclei are shown by DAPI staining in blue and FAM-labeled anti–miR-155 in green. Scale bar indicates 100 μm. (C) Distribution of FAM-labeled anti–miR-155 in BM, spleen, and liver as measured by flow cytometry. Statistical analysis of flow cytometry results is shown in the lower panel in bar graph. Data are shown as means ± SD. **P < .01. (D) Seven SCID mice were dosed with a single tail-vein injection of 25 mg/kg of FAM-labeled anti–miR-155 or saline immediately after injection of mCherry-Luc+-BCWM1 cells. Distribution of FAM-labeled anti–miR-155 in cells from the organs of mice was detected by immunofluorescent imaging and data from 3 representative mice are shown. Cell nuclei are shown by DAPI staining (blue), mCherry-Luc+-BCWM1 cells in red, and FAM-labeled anti–miR-155 in green. Scale bar indicates 100 μm.
Distribution of FAM-labeled anti–miR-155 in mice. Balb/c mice were dosed with a single tail-vein injection of 25 mg/kg of FAM-labeled anti–miR-155 or saline. (A) Distribution of FAM-labeled anti–miR-155 in cells from mice calvarium BM shown by live in vivo confocal microscopy imaging. Blood vessels are shown by Evans blue staining in red and FAM-labeled anti–miR-155 in green. (B) Distribution of FAM-labeled anti–miR-155 in cells from mice organs shown by immunofluorescent imaging. Cell nuclei are shown by DAPI staining in blue and FAM-labeled anti–miR-155 in green. Scale bar indicates 100 μm. (C) Distribution of FAM-labeled anti–miR-155 in BM, spleen, and liver as measured by flow cytometry. Statistical analysis of flow cytometry results is shown in the lower panel in bar graph. Data are shown as means ± SD. **P < .01. (D) Seven SCID mice were dosed with a single tail-vein injection of 25 mg/kg of FAM-labeled anti–miR-155 or saline immediately after injection of mCherry-Luc+-BCWM1 cells. Distribution of FAM-labeled anti–miR-155 in cells from the organs of mice was detected by immunofluorescent imaging and data from 3 representative mice are shown. Cell nuclei are shown by DAPI staining (blue), mCherry-Luc+-BCWM1 cells in red, and FAM-labeled anti–miR-155 in green. Scale bar indicates 100 μm.
We also investigated whether the anti–miR-155 compound could be effectively delivered into WM cells in vivo. To this end, 7 SCID mice per group were engrafted with 3 × 106 mCherry-Luc+-BCWM1 cells, followed by a single IV tail-vein injection of 25 mg/kg of FAM-labeled anti–miR-155 or saline. Two weeks after injection, mouse femoral BM and spleens were collected for immunofluorescence imaging and, as shown in Figure 2D, our results indicate that FAM-labeled anti–miR-155 could be taken up by engrafted WM cells in the BM and spleens of recipient mice.
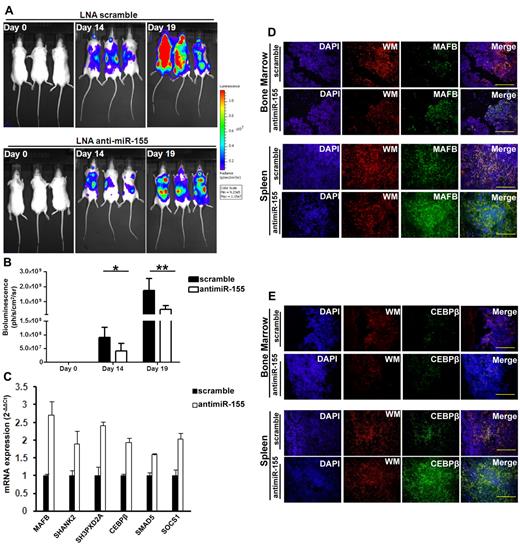
Inhibition of miR-155 decreases tumor growth in a xenograft mouse model of WM
To assess the antitumor activity of anti–miR-155 in vivo, we used a xenograft mouse model of WM. Six SCID mice per group were engrafted with 3 × 106 mCherry-Luc+-BCWM1 cells, after which time mice were injected with a loading dose of 25 mg/kg of anti–miR-155 or scramble control, followed by weekly maintenance doses of 5 mg/kg of each respective compound until the mice were killed. Tumor burden was monitored using bioluminescent imaging at days 0, 14, and 19 after injection (Figure 3A). Image analysis showed that there was a significant reduction in tumor burden at days 14 and 19 in the anti–miR-155–treated mice compared with mice treated with the scramble control (Figure 3B). No difference in body weight was identified between the 2 groups (data not shown).
Inhibition of miR-155 decreases tumor growth in a xenograft mouse model of WM. Immediately after injection of mCherry-Luc+-BCWM1 cells, 6 SCID mice per group were injected with a loading dose of 25 mg/kg of anti–miR-155 or scramble control, followed by weekly maintenance doses of 5 mg/kg of anti–miR-155 or scramble control until mice were killed. (A) Bioluminescent imaging of tumor burden from mice injected with mCherry-Luc+-BCWM1 cells at day 0, 14, or 19. (B) Treatment with the anti–miR-155 decreased tumor burden significantly compared with scramble control as evaluated by whole body imaging. Three representative mice from each group are shown. P = .024 at day 14; P = .009 at day 19 (n = 6 per group). Data are shown as means ± SD. *P < .05; **P < .01. (C) mRNA levels of miR-155 targets were detected by qRT-PCR in the BM CD19+ cells from mice treated with anti–miR-155 or LNA scramble control. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. (D-E) Protein levels of the miR-155 target genes MAFB (D) and CEBPβ (E) were detected by immunofluorescent imaging from the femur BM or spleens of mice. Cell nuclei are shown by DAPI staining in blue; mCherry-Luc+-BCWM1 cells in red. MAFB or CEBPβ proteins were detected by immunostaining with anti-MAFB or anti-CEBPβ. Scale bar indicates 100 μm.
Inhibition of miR-155 decreases tumor growth in a xenograft mouse model of WM. Immediately after injection of mCherry-Luc+-BCWM1 cells, 6 SCID mice per group were injected with a loading dose of 25 mg/kg of anti–miR-155 or scramble control, followed by weekly maintenance doses of 5 mg/kg of anti–miR-155 or scramble control until mice were killed. (A) Bioluminescent imaging of tumor burden from mice injected with mCherry-Luc+-BCWM1 cells at day 0, 14, or 19. (B) Treatment with the anti–miR-155 decreased tumor burden significantly compared with scramble control as evaluated by whole body imaging. Three representative mice from each group are shown. P = .024 at day 14; P = .009 at day 19 (n = 6 per group). Data are shown as means ± SD. *P < .05; **P < .01. (C) mRNA levels of miR-155 targets were detected by qRT-PCR in the BM CD19+ cells from mice treated with anti–miR-155 or LNA scramble control. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. (D-E) Protein levels of the miR-155 target genes MAFB (D) and CEBPβ (E) were detected by immunofluorescent imaging from the femur BM or spleens of mice. Cell nuclei are shown by DAPI staining in blue; mCherry-Luc+-BCWM1 cells in red. MAFB or CEBPβ proteins were detected by immunostaining with anti-MAFB or anti-CEBPβ. Scale bar indicates 100 μm.
We next quantified the mRNA levels of 6 miR-155 targets in the BM WM CD19+ cells by qRT-PCR, which showed that all 6 targets were derepressed after treatment with the anti–miR-155 compared with scramble control (Figure 3C). Moreover, immunostaining confirmed derepression of the MAFB and CEBPβ targets at the protein level in the BM and spleens on treatment with the anti–miR-155 (Figure 3D). These data imply that anti–miR-155–mediated silencing of miR-155 in a xenograft mouse model of WM leads to derepression of direct miR-155 targets in the BM WM CD19+ cells and decreases the tumor growth in recipient mice.
Inhibition of miR-155 decreases WM and CLL proliferation in the context of the BM microenvironment
To examine the effect of anti–miR-155 on tumor progression in the context of the microenvironment, we first quantified the miR-155 levels in BM stromal cells (mesenchymal stem cells) from WM patients compared with normal healthy donors. We found that miR-155 levels in WM stromal cells were higher compared with healthy donor BM stromal cells (Figure 4A). Therefore, we used 20μM anti–miR-155 or scramble control to coculture BCWM1 or MEC1 cells with primary WM BM stromal cells and then assessed cell proliferation by MTT and [H]3 thymidine uptake assays, respectively, after 48 hours. Our results indicate that anti–miR-155 treatment could not only decrease tumor cell proliferation, but also overcame the protective effect induced by coculture of tumor cells with BM stromal cells (Figure 4B). We observed no effect on cell cytotoxicity on stromal cells (data not shown).
miR-155 inhibition decreases WM and CLL proliferation in the context of the BM milieu. (A) qRT-PCR analysis of miR-155 levels in WM stroma (n = 10) compared with normal stroma (n = 3). Data are shown as means ± SD. **P < .01. (B) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours, followed by coculture with stromal cells from WM patients. Cell proliferation was evaluated by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (C) BCWM1 or MEC1 cells were cocultured with stromal cells from wild-type or miR-155−/− mice, and cell proliferation was measured by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. **P < .01. (D) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours, followed by cocultured with stromal cells from wild-type or miR-155−/− mice. Cell proliferation was measured by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01.
miR-155 inhibition decreases WM and CLL proliferation in the context of the BM milieu. (A) qRT-PCR analysis of miR-155 levels in WM stroma (n = 10) compared with normal stroma (n = 3). Data are shown as means ± SD. **P < .01. (B) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours, followed by coculture with stromal cells from WM patients. Cell proliferation was evaluated by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (C) BCWM1 or MEC1 cells were cocultured with stromal cells from wild-type or miR-155−/− mice, and cell proliferation was measured by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. **P < .01. (D) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours, followed by cocultured with stromal cells from wild-type or miR-155−/− mice. Cell proliferation was measured by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01.
Because the BM microenvironment plays a critical role in supporting tumor cell growth, in the present study, we sought to examine the role of miR-155 in tumor proliferation specifically in BM stromal cells. BCWM1 or MEC1 cells were cocultured with BM stromal cells from miR-155–knockout (miR-155−/−) mice or wild-type mice as a control. Cell cytotoxicity and cell proliferation were assessed after 48 hours of coculture. The stromal cells from miR-155−/− mice inhibited the proliferation of BCWM1 and MEC1 cells significantly compared with stromal cells from wild-type mice, indicating that miR-155 may also play an important role in the surrounding microenvironmental cells, lending significant support to tumor growth and proliferation (Figure 4C).
To further clarify whether anti–miR-155 can affect both tumor cells and stromal cells, we treated BCWM1 or MEC1 cells with anti–miR-155 or scramble control, followed by coculturing of the treated cells with BM stromal cells from wild-type mice compared with stromal cells from miR-155−/− mice. Cell survival and cell proliferation were assessed by MTT assay and [H]3 thymidine uptake assays, respectively, after 48 hours of coculture. Our data showed that treatment with anti–miR-155 could decrease tumor cell proliferation compared with scramble control when cocultured with wild-type mice stroma, but not significantly on coculturing with miR-155−/− stromal cells, indicating that anti–miR-155 treatment leads to a similar effect on WM as the genetic miR-155 loss-of-function (Figure 4D).
Discussion
miR-155 acts as an onco-miR in many malignancies, especially B-cell lymphoproliferative disorders. Previous studies have shown that miR-155 is a major regulator of oncogenesis in aggressive and low-grade lymphomas.12,13 However, studies reporting on therapeutic targeting of miR-155 in mouse lymphoma models in vivo have been lacking. In the present study, we used a fully LNA-modified 8-mer anti–miR-155 to inhibit miR-155 function in cultured WM and CLL cells in vitro and in a mouse xenograft model of WM. Our data showed that systemic delivery of the anti–miR-155 resulted in uptake of the compound in the BM, livers, and spleens of mice. The anti–miR-155 compound was also detected in WM cells in the BM and spleens of engrafted recipient mice. Pharmacologic inhibition of miR-155 by systemically delivered anti–miR-155 in a xenograft mouse model of WM resulted in derepression of several direct miR-155 targets in the BM WM CD19+ cells and decreased the tumor growth significantly in recipient mice.
Previous studies have identified several direct targets of miR-155, including SOCS1, FOXO3A, AICDA, PTEN, AGTR1, SMAD5, SHIP1, PU.1, and CEBPβ.27–36 With the aim of understanding which of the aforementioned targets play a role in the pathogenesis of low-grade B-cell lymphomas, in the present study, we carried out GEP in WM cells and found that 3 known miR-155 targets, SMAD5, SOCS1, and CEBPβ, as well as 3 novel miR-155 targets, MAFB, SHANK2, and SH3PXD2A, were derepressed after anti–miR-155 treatment. MAFB belongs to the MAF family of basic leucine zipper transcription factors.37 Combined deficiency for the transcription factors MAFB and c-Maf enables self-renewal of differentiated functional macrophages.38 Maf genes, including MAFB, are mostly bona fide oncogenes, as highlighted by studies from their initial isolation to their involvement in human cancer.39 For example, in humans, Maf genes are overexpressed in approximately 60% of human angioimmunoblastic T-cell lymphomas40 and in approximately 50% of multiple myeloma cases, in which they contribute directly to cancer progression.41–43 However, Maf proteins can be either pro- or antioncogenic, depending on the cell context, and their antioncogenic activity has been linked to their strong terminal differentiating activity.44 Therefore, it is tempting to speculate that miR-155 controls cell proliferation through MAFB and that MAFB may function as a tumor suppressor in B-cell malignancies, because the expression level of MAFB in lymphoma was found to be lower compared with normal cells. However, further studies are needed to elucidate the role of MAFB, SHANK2, and SH3PXD2A in lymphoma and to shed light on the molecular complexity of the miR-155 pathway in these diseases.
The BM microenvironment, which includes nonmalignant bystander cells and secreted cytokines, plays a crucial role in the pathogenesis of nonHodgkin lymphomas.45–47 In the present study, we found higher miR-155 levels in the stromal cells of patients with WM compared with those from healthy subjects (Figure 4A). Interestingly, loss of miR-155 in the stroma led to significant inhibition of tumor growth, indicating that miR-155 regulates tumor proliferation not only when it is overexpressed in the malignant cells, but also when it is present in BM microenvironmental cells (Figure 4). The high level of miR-155 in stromal cells and its regulation of tumor growth are intriguing. Recent studies have shown that exosomes could mediate the transfer of mRNAs and miRs as a novel mechanism of genetic exchange and regulation between cells.48 Future studies are needed to examine the possible exchange of miRs between stromal cells and tumor cells and the mechanisms through which the lack of miR-155 in the stroma regulates tumor growth.
In the present study, we used an 8-mer seed-targeting anti–miR-155 to inhibit miR-155 function in low-grade B-cell lymphomas that harbor high levels of miR-155. Our results indicate that systemically delivered anti–miR-155 antagonizes miR-155 effectively in vivo within the BM microenvironment and other hematopoietic tissues and inhibits tumor growth in a mouse xenograft model of WM in vivo. The results of the present study highlight the potential of the tiny 8-mer anti–miR-155 in therapeutic targeting of miR-155 in hematologic malignancies with aberrant expression of miR-155.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported in part by research grants from the Leukemia & Lymphoma Society, The Kirsch Laboratory for Waldenstrom, and the Heje Fellowship. mCherry-Luc+-BCWM1 cells were a kind gift from Dr Andrew Kung (Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA).
Authorship
Contribution: Y.Z., A.M.R., and I.M.G. designed and performed the research, analyzed the data, and wrote the manuscript; C.R., L.F. S.O., S.M.F., A.S., Y.L., H.N., P.Q., A.K.A., F.A., P.M., and M.R. performed the research; and J.R.B., T.-H.T., and S.K. analyzed the data and edited the manuscript.
Conflict-of-interest disclosure: S.O. and S.K. are employees of Santaris Pharma. I.M.G. is on the advisory board of Millennium-Takeda and Novartis. The remaining authors declare no competing financial interests.
Correspondence: Irene M. Ghobrial, MD, Department of Medical Oncology, Dana-Farber Cancer Institute, 450 Brookline Ave, Boston, MA, 02115; e-mail: irene_ghobrial@dfci.harvard.edu.

![Figure 1. Identification of novel miR-155 target mRNAs in WM. (A) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours. miR-155 inhibition decreases BCWM1 and MEC1 cell proliferation in vitro as evaluated by the [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (B) BCWM1 cells were treated with anti–miR-155 or scramble control for 48 hours. All of the BCWM1 cell samples were cultured and processed in parallel for total RNA extraction and GEP using Affymetrix GeneChip. Validated targets of miR-155 are shown in a heat map on the left and predicted targets of miR-155 are listed on the right. (C) qRT-PCR analysis of selected miR-155 targets in BCWM1 cells treated with anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (D) Stable HEK293 cell lines overexpressing pre-miR-155 or empty vector as a control were generated by lentiviral infection. Cells were transiently transfected with the reporter plasmid pmirGLO driving luciferase expression with a target gene fragment containing the predicted miR-155 binding site or a mutated binding site as a control. Relative luciferase activity was decreased in miR-155–overexpressing HEK293 cells transfected with plasmids harboring miR-155 target sequences compared with plasmids harboring mutated target sequences. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (E) mRNA levels of miR-155 target genes were detected by qRT-PCR from normal donor blood CD19+ cells, BCWM1 and MEC1 cells, primary WM CD19+ cells, and primary CLL cells. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. (F) mRNA levels of miR-155 target genes were detected by qRT-PCR from primary WM CD19+ cells treated with 20μM anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. (G) mRNA levels of miR-155 target genes were detected by qRT-PCR from primary CLL cells treated with 20μM anti–miR-155 or scramble control for 48 hours. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/120/8/10.1182_blood-2012-02-410647/4/m_zh89991295670001.jpeg?Expires=1768542020&Signature=jKRNDGRShGHSxRfWkWvGXpBz30RPgoji2m2CJ~yXEBpyxJ987ntQy6oM1wRGuOTIJ7jw4T1itlg-gbUwNrSBBOKd6PMpP9oxeM1uy4S5NZhkLr70s~OSVy~6zkiPddPfZTlfekvsmJH75b8v-6Ej-m7x~RdIvVpqKOE00qx6yuwH1g2a2m3wSrddfAv6Qigyp7zM8E1wT5sXCpUEIwSeihLBT~XKDf~o9e9AZvKdVfr93U9lWFfQxYRH9rRTvdjSEH0UnOELFBThUUGut~r8VqI0M1o85YJOFmkHoHFdf-MtGuMhT3RXlw31aFi~sPTpp4Bd-KReSmiAjphkYIPllw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 4. miR-155 inhibition decreases WM and CLL proliferation in the context of the BM milieu. (A) qRT-PCR analysis of miR-155 levels in WM stroma (n = 10) compared with normal stroma (n = 3). Data are shown as means ± SD. **P < .01. (B) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours, followed by coculture with stromal cells from WM patients. Cell proliferation was evaluated by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01. (C) BCWM1 or MEC1 cells were cocultured with stromal cells from wild-type or miR-155−/− mice, and cell proliferation was measured by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. **P < .01. (D) BCWM1 or MEC1 cells were treated with 20μM anti–miR-155 or scramble control for 48 hours, followed by cocultured with stromal cells from wild-type or miR-155−/− mice. Cell proliferation was measured by [H]3 thymidine uptake assay. Experiments were performed in triplicate and repeated 3 times. Data are shown as means ± SD. *P < .05; **P < .01.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/120/8/10.1182_blood-2012-02-410647/4/m_zh89991295670004.jpeg?Expires=1768542020&Signature=2WmsjLYZEmwgBQ34m7ABohPTHbKmXnjP0JxnFNqya5WYHycfMZraHAy~OYq7EICg8Abr8k4Po-dHWq3O2F~BBydlkZeTS8XWa2NtqeruoKEVz~z8dzE34HY1DUC9j343dD2ydBtjT6o6hAtdfoJDKRNrCA7JyA37FcdRvSM0~HPVjlGLtqKVR3LTMqD-BqYsctoSTGUcA6c483mnCPimOXejaRwTZ~lueWx-m4w9k1NbpxLVvHUdDE-B8IiCM83AXi7EAzrKZ1tNmPdPxvIgCorPUhIGXeR6nQRZEDwHKfbowrH3ndYHFBsJJ3bpD5-GbPxwPCJdP1Bxobq~820OzA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
