Key Points
Activated CD8+ T cells are preferentially found in the spleen of ITP patients who are nonresponders to rituximab.
Abstract
The pathogenic role of B cells in immune thrombocytopenia (ITP) has justified the therapeutic use of anti-CD20 antibodies such as rituximab (RTX). However, 60% of ITP patients do not respond to RTX. To decipher the mechanisms implicated in the failure of RTX, and because the spleen plays a well-recognized role in ITP pathogenesis, 12 spleens from ITP patients who had been nonresponders to RTX therapy were compared with 11 spleens from RTX-untreated ITP patients and 9 controls. We here demonstrate that in RTX-nonresponder ITP patients, preferential Th1 and Tc1 T lymphocyte polarizations occur, associated with an increase in splenic effector memory CD8+ T-cell frequency. Moreover, in the RTX- nonresponder patient group, the CD8+ T-cell repertoire displays a restricted pattern. In the blood, the phenotype of CD8+ T cells before and after RTX treatment is not modified in responders or nonresponders. Altogether, these results demonstrate for the first time an activation of splenic CD8+ T cells in ITP patients who did not respond to RTX and suggest their involvement in platelet destruction in these patients.
Introduction
Immune thrombocytopenia (ITP) is an autoimmune disease characterized by a low platelet count that increases bleeding risk. Both an immune peripheral destruction of platelets and an insufficient bone marrow production are involved in its pathogenesis.1 B cells play a key role in the disease by producing antiplatelet autoantibodies that target the membrane glycoproteins GPIIb/IIIa, GPIb/IX, and GPIa/IIa.2 The opsonized platelets are then eliminated by macrophages, preferentially in the spleen. The autoantibodies have undergone a class switch and somatic mutations, which requires B- and T-cell cooperation.3 T lymphocytes in ITP patients display specific features, with a cytokine pattern skewed toward a Th1 profile,4-6 an oligoclonal T-cell receptor (TCR) restriction,5,7 and an engagement into antiapoptotic pathways.5 CD8+ T lymphocytes (CTL) could participate to the peripheral destruction of platelets and to the reduced megakaryocyte maturation.8-11 An increase in Fas ligand, granzymes, and perforin expression by CD8+ T cells has been shown, and high soluble granzyme levels have also been detected in the plasma of some ITP patients.8 Previous studies have indicated that regulatory T cells (Treg) are deficient, both in the blood and the spleen of ITP patients.12,13 More recently, a decrease in circulating CD19+CD24hiCD38hi B cells and in the overall production of interleukin 10 (IL-10) by B cells has also been reported, consistent with a regulatory B-cell deficiency.14 Besides peripheral platelet destruction, an impairment in platelet production is also observed, secondary to low thrombopoietin levels15 and to an immune response directed against megakaryocytes, mediated by both CD8+ T cells16 and anti-platelet autoantibodies.17
Different strategies have been considered for the treatment of ITP.18,19 Steroids are the first-line therapy and induce a systemic and profound immunosuppression. Different mechanisms of action have been described for intravenous immunoglobulins (IVIgs), such as blockade of activating Fcγ receptors, increased expression of the inhibitory receptor FcγRIIb, saturation of neonatal Fc receptor, decrease in proinflammatory cytokine production, and promotion of tolerogenic dendritic cell generation.20 However, the effects of IVIg administration lead to only a transient response.18,19 Despite its elusive mechanisms of action, dapsone leads to a prolonged response in 28% of ITP patients.21 Up to now, the treatment that allows the highest long-term response rate remains splenectomy that results in the elimination of splenic macrophages and possibly corrects the immune dysregulations associated with ITP.22 Immunosuppressive drugs that inhibit both T and B cells are now rarely used and reserved to refractory patients.18,19 To increase bone marrow platelet production, thrombopoietin mimetics have been used and lead to high response rates in most patients, but their effects are generally not curative.23,24 Finally, like in many other autoimmune diseases involving B lymphocytes,25 rituximab (RTX) has also shown efficacy in ITP, with 1-, 2-, and 5-year response rates of 40%, 30%, and 20%, respectively.26,27 RTX is a chimeric monoclonal antibody targeting CD20, which is expressed by the B-cell lineage except by pro-B cells and plasma cells. The binding of RTX to CD20 triggers B-cell depletion by different mechanisms, including their immune mediated clearance by complement dependent cytotoxicity, antibody dependent cytotoxicity, and phagocytosis, but also by triggering their apoptosis.25,28 Following RTX administration, a rapid and complete depletion of circulating B cells is observed. Previous reports have shown that response to RTX is associated with a correction of T-cell abnormalities such as the Th1 and Tc1 skewed polarizations, TCR restriction repertoire,5 and Treg deficiency.12 On the other hand, we have shown that failure to respond to RTX was associated with the persistence of splenic plasma cells producing anti-platelet antibodies29 and to an imbalance between effector and regulatory T cells in the spleens of ITP patients who do not respond to RTX, consistent with an increase in the Th1/Treg ratio.13 We thus hypothesized that such an imbalance may foster CD8+ T-cell stimulation leading to an enhanced CTL-mediated platelet destruction that may explain the lack of response to RTX in some patients. To address this hypothesis, splenic cytotoxic T-cell phenotype, polarization, and TCR spectratyping were studied for the first time in ITP patients previously treated or not with RTX and compared with controls.
Materials and methods
Patients
ITP patients, admitted to the University Hospital of Dijon, Dijon, France, were enrolled in this observational study after giving written informed consent in accordance with the Declaration of Helsinki. The study was approved by the institutional review board and the ethics committee of the University Hospital of Dijon. The main inclusion criterion was primary immune thrombocytopenia, ie, a platelet count <100 × 109/L with exclusion of secondary causes such as familial, viral, drug-induced, or other autoimmune-disease–related thrombocytopenia. Treatments were initiated when platelet count was <30 × 109/L and/or bleeding symptoms were observed, as recommended.18,19 Most of the patients were treated with steroids for 3 to 4 weeks and, if necessary, IVIg as first-line therapies, followed by dapsone. RTX and splenectomy were used as second-line therapies at least 6 months and 1 year after the disease onset, respectively, except for a few patients for whom bleeding symptoms were unresponsive to first-line therapies. Patients were considered nonresponders to RTX if their platelet count remained <30 × 109/L 8 weeks after the first RTX administration or if the long-term use of another treatment was mandatory. The spleens of 23 ITP patients were obtained, among which 11 did not receive RTX before splenectomy and were referred to as RTX-untreated patients, when the remaining 12 did not improve after RTX treatment, and were referred to as RTX nonresponders. Characteristics of the splenectomized ITP patients are reported in Table 1. Because the response to splenectomy tends to be lower in patients >60 years,22,30,31 RTX was preferentially used in older patients to avoid surgery, resulting in a higher median age for RTX nonresponders (74.5 [53.8-80]) compared with RTX-untreated patients (27.5 [21.4-46.3]) and controls (28.2 [20.9-63.7]). The control spleens (n = 9) were obtained from posttraumatic splenectomy, except for 1 patient suffering from spherocytosis. Peripheral blood mononuclear cells (PBMC) of 30 ITP patients were collected before the first RTX infusion and compared depending on the response to RTX and with 8 healthy volunteers. Patients were recruited in the University Hospital of Dijon (n = 20) and in the Reference Center for Auto-Immune Cytopenia, University Hospital of Créteil (n = 10) after they gave a written informed consent. Their characteristics are summarized in supplemental Table 1. Samples were also obtained 2 months after RTX infusion for 18 out of 20 patients treated in Dijon. All the experiments were performed in Dijon.
Spleen preparation
The spleens were obtained from ITP patients during scheduled surgery allowing their management within 1 hour after removal. Posttraumatic spleens were stored for 12 hours or less at 4°C until processing. Splenocytes were obtained as previously described13 and stored in liquid nitrogen until their use. After thawing, cell viability was measured over 90% in all cases by using trypan blue exclusion.
Antibodies
The following antibodies were used for flow cytometry (FCM) analysis of lymphocyte subsets: anti-CD19 allophycocyanin (APC), anti-CD27 phycoerythrin (PE)-Cy7, anti-CD28 APC, anti-CD45RA PE-Cy7, anti-CD62L PE, anti-perforin PE, anti–interferon-γ (IFN-γ) APC, anti-IL-4 fluorescein isothiocyanate, anti–IL-17 PE (eBioscience), anti-CD3 PE-Cy7, anti-CD8 Pacific blue, anti-Granzyme B AF647, anti–HLA-DR fluorescein isothiocyanate, and anti-CCR7 AF647 (BD Biosciences). FCM experiments were performed and analyzed in the cytometry platform facility at IFR 100 Santé STIC, University of Burgundy. Data were acquired on a BD Biosciences LSRII cytometer and analyzed with FlowJo software.
For immunochemistry, anti-CD8, anti-CD4, anti–IFN-γ and anti-CD61 (Dako, Glostrup, Denmark) antibodies were used. Staining was performed using a BenchMark Ultra instrument (Ventana Medical Systems, Roche Diagnostic). Diaminobenzidine (DAB) and Ultra Red (Ventana Medical Systems) were used for staining visualization.
Intracellular cytokine staining
Splenocytes or PBMC (1 × 106 cells) were cultured in 24-well plates in 1 mL of RPMI 1640 (Bio Whittaker) with 10% fetal bovine serum (Gibco BRL) and stimulated with 0.1 µg/mL phorbol 12-myristate 23-acetate (PMA), and 1 µg/mL ionomycin (Sigma-Aldrich). Brefeldin A (BD Golgi Plug; BD Biosciences) was added at 1 µL/mL to block cytokine secretion. After 4 hours, the cells were harvested for CD3 and CD8 membrane staining. After fixation and permeabilization (Fixation Permeabilization buffer; eBioscience), intracellular cytokine staining for IFN-γ, IL-17, and IL-4 was performed. Cell subsets were defined as follows: Tc1: CD3+CD8+IFN-γ+, Tc2: CD3+CD8+IL-4+, Tc17: CD3+CD8+IL-17+, Th1: CD3+CD8−IFN-γ+, Th2: CD3+CD8−IL-4+, Th17: CD3+CD8−IL-17+.
CD8+ T-cell isolation
Splenocytes were stained with an anti-CD8 antibody coated with magnetic beads following the manufacturer’s instructions (Miltenyi) and sorted using an AutoMACS device. The mean purity evaluated by FCM was 94%.
Real-time polymerase chain reaction and TCR Vβ spectratyping
Sorted splenic CD8+ T cells were collected in RLT lysis buffer (Qiagen) to further isolate total RNA. After reverse transcription, complementary DNA was amplified with primers specific for IFN-γ, IL-4, IL-17A, perforin, and granzyme B transcripts. Results were normalized to the expression of the ribosomal protein L32. Primer sequences are reported in supplemental Table 2.
For TCRVβ spectratyping, reverse transcription was performed using the SuperScript VILO cDNA Synthesis Kit (Life Technologies). The complementary DNA was then amplified in 24 separate polymerase chain reactions using 24 TCRBV forward specific primers and 1 reverse TCRBC primer as described previously.32 Fluorescent polymerase chain reaction products were run on an ABI377 analyzer to determine CDR3 size length of TCRBV transcripts, and spectratyping profiles were constructed using the Immunoscope 3.1a Software. Fluorescent intensity raw data of each peak in each TCRBV subfamily were collected, and repertoire perturbation index was calculated using the ISEApeaks software.33 For this analysis, peak areas of each TCRBV were compared for their distribution and intensities to an unskewed repertoire. The higher the perturbation index, the more the repertoire is skewed. The nomenclature of TCRBV segments proposed by Arden et al34 was used in this study.
Statistical analysis
Kruskal-Wallis and Mann-Whitney U tests were used to compare quantitative data, as appropriate. Wilcoxon’s signed-rank test was used to compare paired value. Fisher’s exact test was used for qualitative data. Spearman’s rank correlation test was used for correlation analyses. Unless specified, results are given by median (interquartile range). Results were considered statistically significant when P < .05. Analyses were performed on GraphPad Prism.
Results
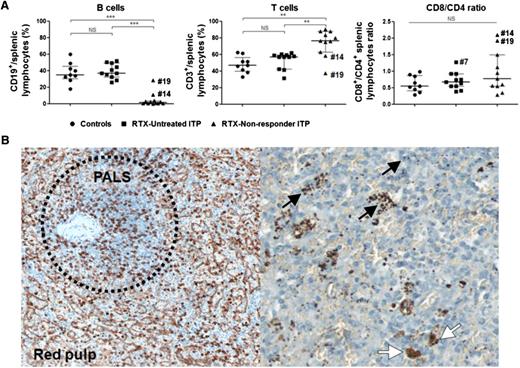
Rituximab depletes splenic B cells but does not modify the CD4+ to CD8+ T lymphocyte ratio
The effect of RTX on splenocytes was determined by comparison of controls (n = 9), RTX-untreated ITP patients (n = 11), and RTX-nonresponder ITP patients (n = 12). RTX-nonresponder ITP patients were splenectomized after a median of 7.1 months (range, 2.3-14.7) after RTX administration. Both RTX-untreated and nonresponder ITP patients exhibited active disease before splenectomy, with a median lowest platelet count during the previous 3 months of 22.5 × 109/L (17.3-27.3) and 14 × 109/L [(6.8-19.5), respectively (Table 1). As expected, a B-cell depletion was obtained in nearly all patients treated with RTX (1.4% [0.3-3.4]), the percentage of B cells representing about 35% of total splenic lymphocytes in both controls (P = .0002) and RTX-untreated patients (P < .0001; Figure 1A). Consequently, the relative amount of T cells among total splenic lymphocytes was increased in RTX nonresponders (Figure 1A) compared with untreated patients (P = .002) and controls (P = .003). B- and T-cell percentages were not correlated with patient age (supplemental Table 3). Patient #19 displayed a high percentage of splenic B cells, which is consistent with B-cell regeneration because the splenectomy was performed 14.7 months after RTX treatment. The percentage of CD8+ T cells among total T lymphocytes, represented by the CD8+/CD4+ ratio, was not different among the 3 groups (Figure 1A). Only 2 out of 12 patients within the RTX-nonresponder group displayed a high CD8+/CD4+ ratio (patients #14 and #19). In both controls and ITP patients, histologic analyses indicated that CD8+ T cells were preferentially localized in the red pulp and, to a lesser extent, in the periarteriolar lymphoid sheaths (Figure 1B). Platelets were also located in the red pulp, at the close vicinity of CD8+ T cells (Figure 1B).
Effect of RTX on splenic lymphocytes and CD8+localization. (A) Splenic lymphocyte subsets were compared among controls (black circles, n = 9), RTX-untreated ITP patients (black squares, n = 11), and RTX-nonresponder ITP patients (black triangles, n = 12). Data representing the percentage of B cells (CD19+), T cells (CD3+), and the cytotoxic/helper T-cell ratio (CD8+/CD4+) are summarized in dot plots. The horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U test. **P < .01; ***P < .001. NS, nonsignificant. (B) On immunohistochemistry analyses, CD8+ T cells were preferentially located in the red pulp (left panel, anti-CD8, DAB, magnification ×400) and also in periarteriolar lymphoid sheaths (PALS) (left panel, within the dashed circle). Platelets were found in the red pulp (black arrows, right panel, anti-CD61, Ultra-Red, magnification ×800) and into macrophages (white arrows). Representative immunohistochemistry of 1 RTX-nonresponder ITP patient.
Effect of RTX on splenic lymphocytes and CD8+localization. (A) Splenic lymphocyte subsets were compared among controls (black circles, n = 9), RTX-untreated ITP patients (black squares, n = 11), and RTX-nonresponder ITP patients (black triangles, n = 12). Data representing the percentage of B cells (CD19+), T cells (CD3+), and the cytotoxic/helper T-cell ratio (CD8+/CD4+) are summarized in dot plots. The horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U test. **P < .01; ***P < .001. NS, nonsignificant. (B) On immunohistochemistry analyses, CD8+ T cells were preferentially located in the red pulp (left panel, anti-CD8, DAB, magnification ×400) and also in periarteriolar lymphoid sheaths (PALS) (left panel, within the dashed circle). Platelets were found in the red pulp (black arrows, right panel, anti-CD61, Ultra-Red, magnification ×800) and into macrophages (white arrows). Representative immunohistochemistry of 1 RTX-nonresponder ITP patient.
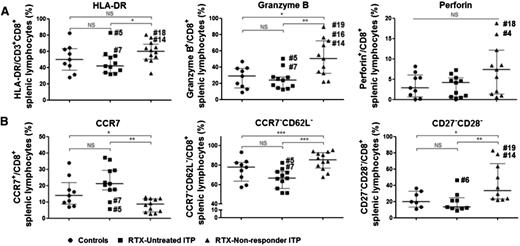
Splenic effector memory CD8+ T cells are increased in patients in whom RTX therapy failed
To study the possible role of splenic CD8+ T cells in ITP pathogenesis, the expression of activation and memory markers, effector molecules involved in the cytotoxic function of these cells, chemokine receptors, and the cytokine production profile of CD8+ T lymphocytes were assessed. In RTX nonresponders, the expression of HLA-DR by CD8+ T cells was increased (60% [50.6-68.9]) in comparison with untreated patients (41.8% [33.7-54.2]; P = .02; Figure 2A) and did not correlate with patient age (supplemental Table 3). Similarly, granzyme B expression by CD8+ T cells was significantly higher in RTX nonresponders (50.3% [32.2-72.3]) than in untreated ITP patients (23.9% [14.4-27.7]; P = .006) and in controls (28.9% [14.6-38.6]; P = .02; Figure 2A). The percentage of granzyme B+ CD8+ T cells positively correlated with patient age in the RTX-untreated group (r = 0.6, P = .04; supplemental Table 3), but not in the control group or in RTX-nonresponder group. Perforin expression was slightly higher in the RTX-nonresponder group than in other groups, although this difference was not statistically significant (Figure 2A). These results were confirmed by gene expression analyses of nonstimulated CD8+ T cells, granzyme B messenger RNA expression being increased in RTX-nonresponders only (Table 2). The expression of CCR7, a chemokine receptor that drives lymphocyte migration into T-cell areas, was also assessed. In RTX nonresponders, CCR7 expression was lower (8.6% [3.9-12]) than in RTX-untreated patients (21.1% [17.4-29.4], P = .001) and controls (14% [8.6-21.9], P = .03, Figure 2B). Combined with the expression of CD62L, an adhesion molecule involved in the recruitment of T cells into secondary lymphoid organs, we observed an increase in CCR7−CD62L−CD8+ T cells in RTX nonresponders (85.4% [77.1-93.3]) when compared with RTX-untreated ITP patients (66.5% [56.2-73.2]; P = .0009; Figure 2B). Neither CCR7+ nor CCR7−CD62L− percentages within CD8+ T cells were correlated with patient age (supplemental Table 3). In the RTX-untreated group, 2 patients (#5 and #7) displayed low CCR7 and CD62L expression together with a high expression of HLA-DR and granzyme B.
Splenic CD8+T-cell phenotype. Splenic CD8+ T-cell phenotype was characterized for the expression of (A) HLA-DR and the cytotoxic proteins granzyme B and perforin. (B) The expression of the chemokine receptor CCR7, the adhesion molecule CD62L, and the memory markers CD27 and CD28 were also assessed. Data are summarized in dot plots representing the expression of each marker among CD8+ T cells, in 9 controls (black circles), 11 RTX-untreated patients (black squares), and 12 RTX nonresponders (black triangles). The horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U test. *P < .05; **P < .01; ***P < .001. NS, nonsignificant.
Splenic CD8+T-cell phenotype. Splenic CD8+ T-cell phenotype was characterized for the expression of (A) HLA-DR and the cytotoxic proteins granzyme B and perforin. (B) The expression of the chemokine receptor CCR7, the adhesion molecule CD62L, and the memory markers CD27 and CD28 were also assessed. Data are summarized in dot plots representing the expression of each marker among CD8+ T cells, in 9 controls (black circles), 11 RTX-untreated patients (black squares), and 12 RTX nonresponders (black triangles). The horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U test. *P < .05; **P < .01; ***P < .001. NS, nonsignificant.
To distinguish between naïve and late-differentiated T cells, CD27, CD28, and CD45RA expression was analyzed. In RTX-nonresponders, the frequency of CD27−CD28−CD8+ T cells was significantly increased (33.2% [23.3-67.1]) in comparison with RTX-untreated ITP patients (13.4% [11.6-24.9]; P = .004) and controls (19.7% [13.3-32.9]; P = .04; Figure 2D). No correlation between the percentage of CD27−CD28−CD8+ T cells and patient age was observed (supplemental Table 3). Approximately 50% of CD8+ T lymphocytes expressed CD45RA, without difference among the 3 groups (data not shown).
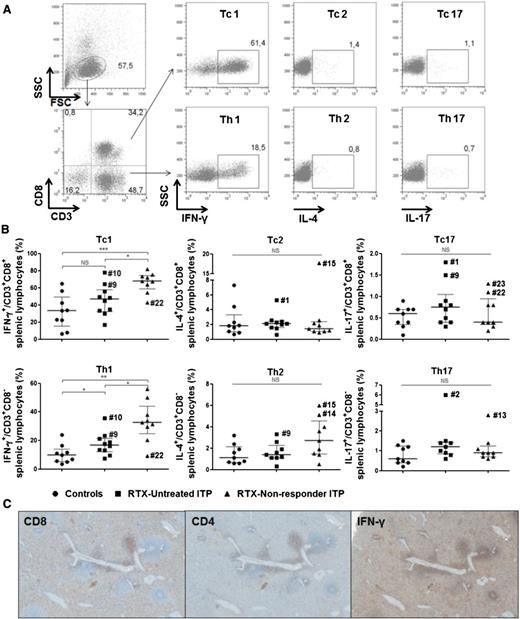
Analysis of the nature of the T-cell lineage commitment indicated an increase in IFN-γ+CD8+ (Tc1 cells) in RTX nonresponders (68% [59.1-81.6]) in comparison with RTX-untreated ITP patients (46.6% [32.3-57.8]; P = .02) and controls (33.3% [15.2-49.2]; P = .0008; Figure 3B). IFN-γ production by CD3+CD8− T cells, which mainly represent Th1 cells, was increased in RTX-nonresponder ITP patients, representing 32.5% [24.8-44] vs 16.8% [12.2-21.7] in RTX-untreated ITP patients (P = .001) and 9.7% (5.3-14) in controls (P = .02; Figure 3B). Th1 percentage did not correlate with patient age (supplemental Table 3). No difference in the production of IL-4 and IL-17 by CD8+ or CD4+ T cells was observed. IFN-γ–producing cells were located by immunochemistry and were consistent with CD8+ and CD4+ T cells (Figure 3C). IFN-γ, IL-4, and IL-17 messenger RNA expression in CD8+ T cells, analyzed without any stimulation, was similar among the 3 groups (Table 2).
Splenic T-cell commitment. Splenocytes were stimulated with PMA and ionomycin in the presence of Brefeldin A for 4 hours. Cells were first stained for CD3 and CD8. After fixation and permeabilization, intracellular staining for IFN-γ, IL-4, and IL-17 was performed. (A) For FCM analyses, lymphocytes were first gated on their forward (FSC) and side scatter (SSC), then on their expression for CD3 and CD8. Cells were defined as Tc1: CD3+CD8+IFN-γ+, Tc2: CD3+CD8+IL-4+, Tc17: CD3+CD8+IL-17+, Th1: CD3+CD8−IFN-γ+, Th2: CD3+CD8−IL-4+, and Th17: CD3+CD8−IL-17+. The results of a representative RTX-nonresponder patient are depicted. (B) Data are summarized in dot plots representing the expression of each cytokine among T cells, in 9 controls (black circles), 10 RTX-untreated patients (black squares), and 9 RTX nonresponders (black triangles). The horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U test. *P < .05; **P < .01; ***P < .001. NS, nonsignificant. (C) IFN-γ–producing cells were located within periarteriolar lymphoid sheath (PALS) and in the red pulp and consist of CD8+ and CD4+ T cells (CD8, CD4, and IFN-γ staining, DAB, magnification ×400). Representative immunohistochemistry of 1 RTX-untreated ITP patient.
Splenic T-cell commitment. Splenocytes were stimulated with PMA and ionomycin in the presence of Brefeldin A for 4 hours. Cells were first stained for CD3 and CD8. After fixation and permeabilization, intracellular staining for IFN-γ, IL-4, and IL-17 was performed. (A) For FCM analyses, lymphocytes were first gated on their forward (FSC) and side scatter (SSC), then on their expression for CD3 and CD8. Cells were defined as Tc1: CD3+CD8+IFN-γ+, Tc2: CD3+CD8+IL-4+, Tc17: CD3+CD8+IL-17+, Th1: CD3+CD8−IFN-γ+, Th2: CD3+CD8−IL-4+, and Th17: CD3+CD8−IL-17+. The results of a representative RTX-nonresponder patient are depicted. (B) Data are summarized in dot plots representing the expression of each cytokine among T cells, in 9 controls (black circles), 10 RTX-untreated patients (black squares), and 9 RTX nonresponders (black triangles). The horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U test. *P < .05; **P < .01; ***P < .001. NS, nonsignificant. (C) IFN-γ–producing cells were located within periarteriolar lymphoid sheath (PALS) and in the red pulp and consist of CD8+ and CD4+ T cells (CD8, CD4, and IFN-γ staining, DAB, magnification ×400). Representative immunohistochemistry of 1 RTX-untreated ITP patient.
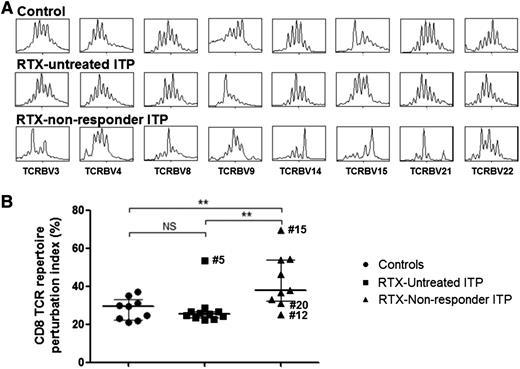
Splenic CD8+ T lymphocytes display an oligoclonal pattern in RTX-nonresponder patients
Spectratype analysis of the different TCR Vβ families of splenic CD8+ T cells was assessed for the first time. This analysis revealed an oligoclonal pattern in RTX nonresponders, as indicated by the reduction of the number of peaks corresponding to the different CDR3 size lengths (Figure 4A). The TCR repertoire displayed significantly more alterations in RTX nonresponders (37.7% [32.2-53.9]) when compared with RTX-untreated ITP patients (25.6% [23.4-26.8]; P = .004) and controls (29.4% [22.3-33]; P = .005). No significant difference was observed between controls and RTX-untreated patients (P = .6; Figure 4B). The higher rate of alterations was observed for TCR Vβ 3, 4, 6a, 9, 18, 21, 22, and 23, allowing the discrimination between RTX-untreated and RTX-nonresponder ITP patients (supplemental Table 3). No correlation was found between age and TCR abnormalities (supplemental Table 3) or with disease duration (data not shown).
CDR3 size analysis of TCR Vβ transcripts from splenic CD8+T cells. CD8+ splenic T cells were sorted to perform CDR3 size length analysis. (A) Results of eight Vβ spectratypes among the 24 analyzed are shown for 1 representative subject in each group (control, RTX-untreated, and RTX-nonresponder ITP patients). (B) CD8+ T-cell TCR repertoire perturbation indexes, calculated using ISEApeaks software, are summarized in dot plots in 9 controls (black circles), 11 RTX-untreated patients (black squares), and 9 RTX nonresponders (black triangles). The horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U test. **P < .01. NS, nonsignificant.
CDR3 size analysis of TCR Vβ transcripts from splenic CD8+T cells. CD8+ splenic T cells were sorted to perform CDR3 size length analysis. (A) Results of eight Vβ spectratypes among the 24 analyzed are shown for 1 representative subject in each group (control, RTX-untreated, and RTX-nonresponder ITP patients). (B) CD8+ T-cell TCR repertoire perturbation indexes, calculated using ISEApeaks software, are summarized in dot plots in 9 controls (black circles), 11 RTX-untreated patients (black squares), and 9 RTX nonresponders (black triangles). The horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U test. **P < .01. NS, nonsignificant.
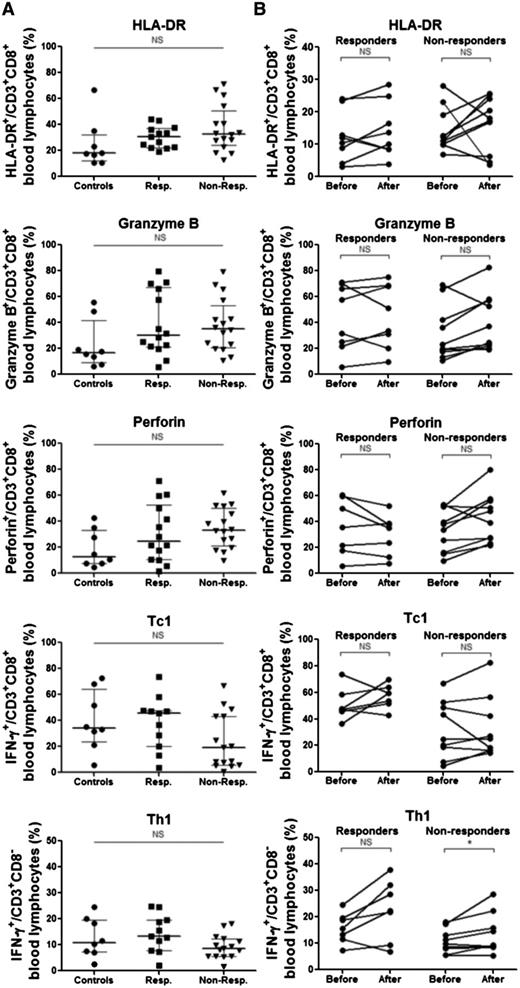
Circulating CD8+ T cells are not altered before or after RTX infusion
To investigate whether circulating CD8+ T cells exhibited the same phenotype as their splenic counterparts, PBMCs from 8 controls and 30 ITP patients, obtained before RTX treatment, were analyzed. ITP patients were retrospectively classified as responders (n = 14) and nonresponders to RTX (n = 16; supplemental Table 1). The expression of HLA-DR, granzyme B and perforin by CD8+ T cells together with the percentages of Tc1 cells were not statistically different among the 3 groups (Figure 5A).
Circulating lymphocytes from controls and ITP patients. (A) PBMCs from 8 controls and 30 ITP patients were assessed. For ITP patients, the samples were obtained before RTX infusion that leads to a response in 14 cases. Flow cytometry was performed to analyze the expression of HLA-DR and the cytotoxic proteins granzyme B and perforin. After a polyclonal stimulation with PMA and ionomycin, intracellular expression of IFN-γ was measured in CD8+ (Tc1) and CD3+CD8− T cells (Th1). (B) The same analyzes were performed in 18 ITP patients before and after RTX treatment, among whom 8 reached a clinical response. Data are summarized in dot plots, and the horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U or Wilcoxon signed-rank tests as appropriate. Non-Resp., nonresponder; NS, nonsignificant; Resp., responder.
Circulating lymphocytes from controls and ITP patients. (A) PBMCs from 8 controls and 30 ITP patients were assessed. For ITP patients, the samples were obtained before RTX infusion that leads to a response in 14 cases. Flow cytometry was performed to analyze the expression of HLA-DR and the cytotoxic proteins granzyme B and perforin. After a polyclonal stimulation with PMA and ionomycin, intracellular expression of IFN-γ was measured in CD8+ (Tc1) and CD3+CD8− T cells (Th1). (B) The same analyzes were performed in 18 ITP patients before and after RTX treatment, among whom 8 reached a clinical response. Data are summarized in dot plots, and the horizontal bar represents the median with the interquartile range. P values were derived by Mann-Whitney U or Wilcoxon signed-rank tests as appropriate. Non-Resp., nonresponder; NS, nonsignificant; Resp., responder.
Because the immune features observed in the spleen after RTX could be linked to the treatment and not to the underlying mechanism of platelet destruction, the effect of RTX on circulating T cells was also investigated in 15 ITP patients by comparing their phenotype just before the first RTX infusion and 2 months later. HLA-DR, granzyme B, perforin, and IFN-γ expression by CD8+ T cells was not different before and after treatment in both responders and nonresponders (Figure 5B). Th1 cells significantly increased after RTX in nonresponders (mean of 10.8 ± 4.6 vs 13.6 ± 7.6, P = .04) but not in responder patients (15.8 ± 5.7 vs 22.7 ± 11.4, P = .08).
Response to splenectomy is not associated with a specific splenic CD8+ T-cell phenotype
To address which factors could influence the response to splenectomy, patient characteristics and the different biological parameters were compared between responder and refractory patients to splenectomy. The analysis was not performed in the RTX-untreated group because only 1 patient out of 11 was not cured by splenectomy. The results are reported in the supplemental Table 5. Overall, refractory patients were older than responders to splenectomy (77.2 [61.4-80.0] vs 42.7 [25.0-56.8]; P = .04). The lowest platelet count during the 3 months before splenectomy was lower in refractory patients (12.5 [5.5-18.5]) compared with responders to splenectomy (21.0 [12.0-27.0]; P = .04). Regarding the splenic immune response, only Tc2 percentage was significantly different between responders (2.1 [1.6-2.6]) and refractory patients (1.1 [0.6-1.3]; P = .003). Neither the Tc1/Tc2 nor the Th1/Th2 ratio was significantly different (data not shown). None of the different parameters was significantly different when considering only the RTX-nonresponder group.
Discussion
The mechanisms involved in the absence of response to RTX in patients with autoimmune diseases such as ITP remain to be defined. We previously reported that the resistance to RTX treatment may be explained by the persistence of splenic plasma cells,13 which was recently confirmed, because long-lived plasma cells represent the major residual cells of the B-cell compartment in the spleen after RTX administration and, therefore, the producers of antiplatelet antibodies.29 However, it is also known in ITP that a clinical response can be achieved despite the persistence of antiplatelet antibodies.35 Because B cells are not only effector cells that produce pathogenic antibodies but also professional APCs, their removal by RTX may also significantly affect T-cell immune response. However, we previously observed an increase in the Th1/Treg ratio13 in the spleen of ITP patients who failed to respond to RTX, which, we hypothesized, may promote the activation of cytotoxic T cells. In the current study, we demonstrate that despite the fact that the splenic CD8+/CD4+ T-cell ratio is not modified in RTX nonresponders compared with RTX-untreated ITP patients and controls, the phenotype of CD8+ T cells is consistent with activated CTL that highly express HLA-DR and granzyme B. In the spleen, CD8+ T cells expressing high levels of CCR7 are attracted into the periarteriolar lymphoid sheaths, whereas CD8+ T cells weakly expressing CCR7 migrate into the red pulp.36 The costimulatory molecules CD27 and CD28 involved in the activation and the proliferation of T cells are less expressed on late differentiated cells.37 In RTX nonresponders, splenic CCR7−CD62L−CD8+ and CD27−CD28−CD8+ T cells are increased, revealing the late-differentiated state of CD8+ T cells localized in the red pulp. Moreover, CD8+ T cells display a restricted TCR repertoire consistent with a chronic stimulation by specific antigens that are most likely platelet-derived antigens in these ITP patients. In accordance with an effector memory T-cell phenotype, CD8+ T cells express high level of granzyme B in RTX nonresponders.37,38 Indeed, a perforinlow granzyme B+ phenotype is observed in late effector memory CD8+ T cells, whereas early effector memory T cells are perforin−/low granzyme B− and central memory T cells are perforin− granzyme B−.39 Also associated with a phenotype of effector memory CD8+ T cells, the secretion of IFN-γ is high in RTX nonresponders, while IL-4 and IL-17 secretions are not different from RTX-untreated ITP patients or controls. This Tc1 polarization is associated with an increase in Th1 cells that is even more important in RTX nonresponders and that is probably involved in the sustained stimulation of splenic CD8+ T cells. Splenic CD8+ T cells of 2 patients (#5 and #7) within the RTX-untreated group showed a high expression of HLA-DR and granzyme B together with a low expression of CCR7. Patient #5 also displayed a high TCR repertoire perturbation index. Because these characteristics were preferentially observed in the RTX nonresponders, one can assume that these 2 patients would have not responded to RTX.
In accordance with a previous report,40 our results argue that the spleen may be the site of platelet destruction by CD8+ T cells because platelets are localized in the cords of the red pulp that are lined by CD8+ T cells.40 Thus, the specific spleen anatomy allows a close contact between cells supporting this cellular immune response. Moreover, the prominent effector memory phenotype associated with the TCR restriction preferentially observed in RTX-nonresponder ITP patients strongly supports the possibility of a CTL-mediated platelet lysis in the spleen of these patients. However, because the response to splenectomy in this cohort of RTX nonresponders is only 58%, other mechanisms such as a CD8+ T-cell immune response against megakaryocytes may also be involved in the pathogenesis of the disease. Indeed, it has been shown that T cells are recruited into the bone marrow of ITP patients41 and that these T lymphocytes are capable of impairing megakaryocyte functions.16 The role of CTL in the reduction of platelet production has also been demonstrated in a murine model of ITP,42 in which megakaryocytes are decreased and display apoptotic features, a type of cell death that is preferentially mediated by cytotoxic lymphocytes. Unfortunately, CD8+ T cells were not assessed in bone marrow biopsy specimens in our study, as bone marrow biopsy is not mandatory in ITP diagnosis and follow-up.18,19
Whether RTX nonresponders exhibit a preferential CD8+ T-cell–mediated disease before the administration of RTX or whether it is directly or indirectly induced by RTX is yet to be determined. To fully address this question, the spleen of RTX nonresponders should be compared with the one of responders, which is not possible because they will not undergo splenectomy. However, the fact that circulating CD8+ T cells before RTX treatment were not significantly different between responders and nonresponders argues for a CD8+ T-cell response restricted to the spleen. Taking into account the clinical heterogeneity of ITP, one can assume that the preferential involvement of CD8+ T cells influences the response to treatments or that some treatments such as B-cell–depleting therapy may unveil their role in ITP pathogenesis. In the aforementioned mouse model, the mechanism underlying platelet destruction affects the efficacy of treatments. Thus, IVIgs are not effective when thrombocytopenia relies on CTL, contrary to B-cell–mediated ITP. In our study, the unresponsiveness to RTX clearly correlates with the activation of splenic CTL.
Because detection of predictive factors to the response to RTX is a critical issue in ITP patients, circulating CD8+ T-cell phenotype before RTX treatment was analyzed. Our results show that circulating CD8+ T-cell activation and polarization do not allow for the distinction between responders and nonresponders to RTX. These results highlight the major role played by the spleen in the autoimmune response during ITP43 and further underline that circulating cells do not fully reflect the immune response that occurs in lymphoid organs or at the site of inflammation. Therefore, identifying predictive factors of treatment success relying on blood parameters may be challenging, although they are particularly needed to optimize the effectiveness of treatments and to rationalize the use of expensive drugs.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by a grant from the Direction de la Recherche Clinique du CHU de Dijon and the Conseil Régional de Bourgogne 2010 (S.A., B.B., and B.L.).
Authorship
Contribution: S.A. and B.B. were the principal investigators; S.A., N.J., and B.B. designed the study; S.A., V.L., S.B., M. Mahévas, M. Michel, B.G., B.S., B.L., and B.B. recruited the patients; S.A., M.S., M.T., N.J., M.C., A.G., F.S., M. Mahévas, L.M., and C.F. performed the experiments; P.O.-D., N.C., and P.R. performed the splenectomies; S.A. and A.S.-F. analyzed the results; S.A., N.J., and B.B. coordinated the research; and S.A., N.L., P.S., N.J., and B.B. wrote the manuscript.
Conflict-of-interest disclosure: S.A. received honoraria from Amgen, GSK, and LFB. The remaining authors declare no competing financial interests.
Correspondence: Bernard Bonnotte, INSERM UMR 1098, Faculté de Médecine, Boulevard Jeanne d’Arc, 21079 Dijon, France; e-mail: bernard.bonnotte@u-bourgogne.fr
References
Author notes
N.J. and B.B. contributed equally to this study.